Women. Do you ever pee a little bit when you do things like cough, sneeze, laugh, or jump? There’s a name for it — stress urinary incontinence. It’s fairly common, but most women keep it to themselves. They’re usually either embarrassed or think it’s just something they have to live with.
Muscles in the floor of the pelvis should be able to prevent urine from leaking when there’s extra pressure on the bladder. If they’re weak they can’t do the job well and that’s why urine leaks out. You might think it’s something that happens to older women who are past menopause, but stress urinary incontinence is actually more common in premenopausal women and is also fairly common in college-aged athletes.
“It’s more likely to occur in postpartum women who’ve had children,” explained Adrienne McAuley, a physical therapist whose specialty is pelvic floor muscle function, “but it can also happen in women and even girls who have not had children. That’s because it really has to do with a muscular imbalance. Sometimes we see it in very high-level athletes who’ve worked a lot on their abdominal muscles but have never heard about their pelvic floor muscles. So they have an imbalance.”
There has been quite a bit of research into the connection between stress urinary incontinence and weak pelvic floor muscles. A growing number of physical therapists, like Adrienne, now specialize in pelvic floor muscle function. “I think there’s a large number of people out there who are living day in and day out with the problem and not realizing how easily treatable it is,” she said. “They need to learn how to use the muscles more effectively, more efficiently. It’s more than doing Kegels, which are pelvic floor muscle contractions. It’s learning how to do them correctly. And for some women, they might not be the right answer. It’s a problem that most women don’t bring up with their health care provider. And generally, not a conversation provider will initiate.”
Weak pelvic floor muscles may be a primary cause of stress urinary incontinence, but Adrienne noticed that a lot of her patients also have problems with their hips — pain or trouble walking correctly, for instance. She believes the two issues may work together to cause the incontinence. There has been some research done, but it’s scant, so she decided to launch her own study.
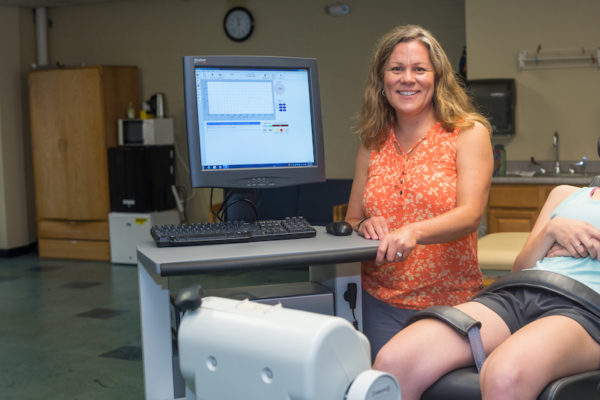
In addition to her clinical practice, she is also on the faculty at the University of New England (UNE). She asked fellow physical therapist and faculty member Erin Hartigan to help her design a study. Erin is a researcher whose expertise is in biomechanics. “In my research, I’ve worked with women who ruptured the anterior cruciate ligament in their knee,” she said. “I try to prevent the injury and also promote restoration of normal movement after reconstructive surgery.”
When Adrienne explained her theory to Erin it got her thinking that weak pelvic floor muscles might be the reason why some of the female athletes she worked with didn’t do well after ACL surgery. She already knew that these women often had trouble controlling their hips. Even though during the initial evaluation she always asked if they had any issues with urine leakage, she realized that most of them said no and that was that. Now she probes a little deeper: “I’ll ask, so you’ve never peed a little bit when you exercise? And that’s when they’ll say, ‘Oh, well, sure, but it’s just a little bit. I just put on a mini pad and I’m fine.’ I’ll say well, that’s stress urinary incontinence and that’s not normal.”
What she discovered was that women she worked with who had musculoskeletal problems in their hips and weren’t doing well after ACL reconstruction also had symptoms of leaking. For their research, which is funded by the American Physical Therapy Association, Adrienne and Erin decided to compare women with stress urinary incontinence to women who are about the same age and doing the same activities but have no symptoms of incontinence. They will look at how their pelvic floor muscles work and how strong and flexible their hips are.
How to participate in the study
The study is currently underway, but they need additional participants. Here are the basic requirements:
- Women 18 and older who have stress urinary incontinence
- May or may not have had children
- Must have a regular menstrual cycle (every 21-35 days)
- Not in pain
- Not have urine leakage that is urge dominant (“gotta go, gotta go”)
- Not have had back or leg surgery
- Not have a body mass index greater than 30 kg/m2
After Adrienne does a physical exam of the hips and pelvic floor muscles (which includes an internal exam), participants will spend most of their time in UNE’s motion analysis lab.
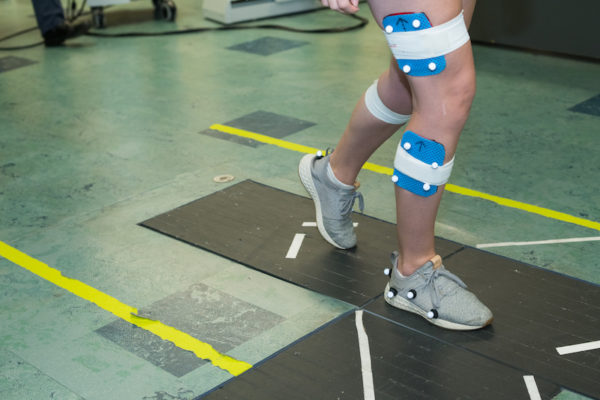
“I’ll put equipment on them and look at how they move, have them walk and do some jumping jacks,” she explained. “Then I’ll have them go to the bathroom, put on a special pad, and drink 16 ounces of water. An hour after drinking, Adrienne will do an external ultrasound to see how full the bladder is and I’ll have them repeat walking and doing jumping jacks. If they pee into the pad, they tell us when. We can then look at their position using the motion analysis equipment. We can also weigh the pad — our equipment is very sensitive — to see how much they leaked.”
The entire session takes about 3 1/2 hours. Participants only have to come once and they get a $100 Amazon gift card. If you are interested in being part of the study, contact Erin Hartigan by email.
If their research does show that hips and pelvic floor muscles are both connected to stress urinary incontinence it might make a world of difference for many women. Physical therapists who specialize in pelvic floor muscle function will know to take a look at hip muscle function as well. Physical therapists who don’t do internal pelvic floor muscle examination and have patients with a weak hip or who have trouble walking will have weak pelvic floor muscles on their radar and can refer to a physical therapist with that expertise.
As an aside, if you are looking for a physical therapist who specializes in pelvic floor muscle health, the American Physical Therapy Association has a handy locator on its website.



Thank you Diane for this very informative article. These are things I never knew as a nurse. It is great to see articles about health problems like this with possible non invasive remedies. Too often surgery is recommended for women with Stress incontinence, and far too often, surgical mesh is used This mesh has messed up the lives of far too many women. The materials are petroleum based, and not accepted well by human tissue. It clumps up, and breaks up and caused multiple issues for women, ruining their lives. Some endure repeated surgical attempts to remove the mesh. Others suffer livelong pain and are unable to have sexual intercourse with their partners. There are other ways to surgically fix a prolapsed uterus or other issues that may cause incontinence. You have describes an excellent intervention for this issue.
This was an article that explains well that not all health problems require a surgical intervention. No risk physical therapy may often be the way to go (no pun intended).
Kathy, thank you so much for your comments, which add another dimension to the story. It’s good to hear from you.