
Luanne Cameron lived with a host of health issues for more than two decades. It wasn’t until after she was diagnosed with DCIS (ductal carcinoma in situ or stage 0 breast cancer) in 2015 that she learned what she believes was at the root of many of her problems.
After her breast cancer diagnosis, she had a mastectomy followed by breast reconstruction surgery. A few months later, she saw her current primary care doctor for a followup. “I had a complete blood workup,” she told me, “and he said everything looked good except I had slightly high calcium. I said no big deal, I’ve had that for 20-25 years. And he said no, you’re not supposed to have a slightly high calcium level and that it might be hyperparathyroidism.”
The news floored Luanne. She remembered when her second child was about a year and a half (he’s 24 now) she went to her previous doctor because she was always crying and it didn’t make sense to her. “My career was taking off,” she said, “I was happily married to my best friend and I was way beyond postpartum blues.”
A blood test showed that her calcium was very high. She was taking extra calcium supplements because her grandmother had osteoporosis and she thought the extra calcium would lower her risk. She went off the supplements and two weeks later her calcium was still high, but only slightly. “My doctor said we’re going to keep an eye on this and I went back to my regular routine,” she explained. “Five years later, it was still slightly high so he said I should go in every year for a physical. Slightly high became my normal.”
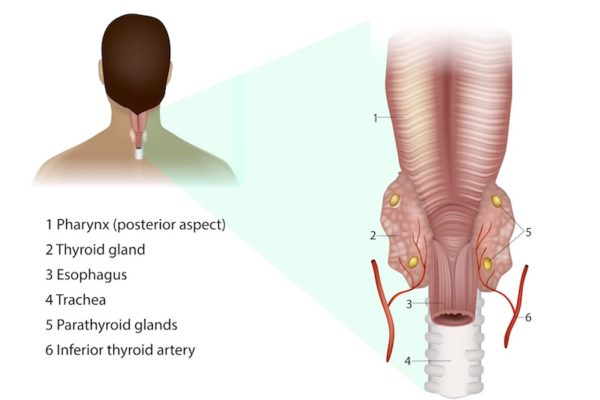
The parathyroid glands
Source: Adobe Stock
The parathyroid glands, which are about the size of a grain of rice, are located in the back of the neck behind the thyroid gland. There are usually four and they sit two to each side. Their purpose is to secrete a parathyroid hormone (PTH) that regulates the amount of calcium we have in our bodies. If any of the four glands secretes too much PTH, calcium levels go up. One of the things that can cause that to happen is a tumor in one of the glands. In most cases, it is a benign or non-cancerous tumor.
The condition is called primary hyperparathyroidism. In the United States, about 100,000 people develop the disorder each year. Women outnumber men two to one. The risk increases with age. An estimated two out of 1000 women 60 or older are diagnosed in the U.S. every year.
Parathyroid glands
It turned out that Luanne, who was in her early 50s, had tumors in two of her parathyroid glands. She also happened to have five glands, but that fact isn’t essential to her story. The surgeon took out the two tumorous glands and left the other three as they were. There were no further treatments.
Dr. Heidi Golden, an endocrinologist affiliated with Maine Medical Center and one of Luanne’s doctors, said hyperparathyroidism is fairly common especially in people as they age but that it can go undetected. “It can take decades for people to have a negative consequence of primary hyperparathyroidism,” she said. “Before calcium levels were drawn frequently we often did not diagnose hyperparathyroidism until people had very elevated levels and obvious symptoms.”
Hyperparathyroid symptoms
About 80% of people with hyperparathyroidism have few or no symptoms and are diagnosed because elevated calcium was noticed on a blood test that was done for some other reason.
“It’s not typical to get significant symptoms until your calcium is that at least one above the upper limit of normal,” said Dr. Golden. “Normal is usually a blood calcium level of 10.3. Anything above that is typically abnormal.”
Luanne told me that one of her doctors used the term “moans, bones, groans and stones” to describe common symptoms related to too much calcium in the blood.
When there are symptoms, the most common are:
- Achy joints
- Fatigue
- Weakness
- Loss of appetite
- Mild depression
- Difficulty concentrating
At higher hormone and calcium levels, which usually happen over the long term, more symptoms can develop:
- Significant loss of appetite
- Nausea
- Constipation
- Excessive thirst
- Frequent urination
- Impaired kidney function
- Kidney stones
- Decreased bone density (osteopenia or osteoporosis)
- Gout
- Hardening of the cartilage in the wrists or knees
- Decreased blood phosphate level
- Slightly increased magnesium level
In rare cases, a person can go into parathyroid crisis. It may happen if they have another illness that causes vomiting and diarrhea and results in a significant loss of fluid, which can lead to very high levels of PTH and calcium. Symptoms include:
- Significant change in thinking and alertness — from confusion to coma
- Severe abdominal pain
- Nausea
- Vomiting
- Stomach Ulcers
- Inflammation of the pancreas
The list of symptoms above came from the website UpToDate.
Treating hyperparathyroidism
“Surgery is the treatment of choice for hyperparathyroidism,” said Dr. Golden. “When we diagnose someone we immediately try to determine whether or not they should have surgery right away or be monitored. Surgery may be recommended if the person:
- Has symptoms
- Has a calcium level one above the upper limit of normal
- Has elevated calcium and osteoporosis or kidney stones
- Has very high levels of calcium in the urine
- Is diagnosed before age 50. (“The presumption,” explained Dr. Golden, “is that you’re going to live many, many more years and probably suffer some complication related to hyperparathyroidism.”)
Luanne didn’t even realize she had any symptoms until after her parathyroid surgery in July 2016. Her calcium level returned to normal and she began to feel better than she had in a long time. If she had known 20+ years ago what she knows now she would have insisted that her doctor do more than monitor her every year. And she certainly wouldn’t have brushed off her slightly high calcium levels as being normal for her.
“I never realized I had slight memory loss and slight anxiety,” she said. “I had built crutches around them. They were immediately gone after the surgery. I never knew I’d been living with them, but now I feel wonderful. Not every story is as extreme as mine. I think it’s because I had it for so long — for more than 25 years. They told me I had super hyperparathyroidism.”
She said she also had severe colitis which has calmed down. Although colitis isn’t listed as a symptom, stomach ulcers and abdominal pain are and she believes there is a connection. She had several other health issues and was seeing multiple specialists. Like the colitis, many were not on the list of common symptoms, but again, she’s convinced her hyperparathyroid disease played a role.
“I put it all together,” she said. “I had 11 different diagnoses and I drew the conclusion that every single one was related to my autoimmune system. I think my elevated calcium was attacking my immune system.”
Whether or not her theory can be proven isn’t really the point. What is important is that life today is much different for Luanne than it was before her diagnosis and surgery. She is determined to make other people aware of the significance of hyperparathyroidism and of a blood test that shows your calcium levels are high, even slightly high. It’s not something to be ignored.
As an aside, Luanne has a philosophy about life (personal and business) that she is also passionate about. She shares it on her website and has written a book that is now in its final edits — she calls it The 110 Philosophy. “My vision is to live to be 110 years young,” she said, “and for me, that means being 110% engaged, no matter what I’m doing. Even when I didn’t feel well, I never looked sick. That’s because I worked so hard to look and feel great. I exercised, drank lots of water, didn’t overeat.”
And how is she feeling these days? Why, 110 %, of course! “I’m truly healthy now,” she told me. “I feel amazing. I thought I was getting old. I thought it was old age. I’m 55 years old now



I had my first kidney stone in 2004 while I was away with my husband while he worked in the DC area. A trip to the ER confirmed that it was a stone and it passed while I was there. I had my second one 5 years later, while my father was dying in a rural nursing home. I ignored it until it passed with a clink in the toilet one morning. Then the final one in 2014 was over a half inch across. That one required removal through cystoscopy and laser lithotrypsy. The pain was the worst of my life. I knew I had elevated calcium levels and PTH Parathyroid hormone levels. It took 3 stones for me to make my decision to have my parathryoid glands removed. All but a tiny part of one gland were removed. I haven’t had a stone since. I didn’t have the dramatic change of generalized symptoms that the author of this story had, but I have not had another kidney stone, and it was worth that alone. I’ve only known a few people who have had this surgery,, but it is always worth it and the recovery is generally very simple.
Kathy, It’s not always easy to decide to have any kind of surgery. Some of my family members have had kidney stones and, like you, told me it was the worst pain they’d ever had. I’m glad you haven’t had another! Thanks for sharing your story with us. I’m sure it will help someone else.
After 15 months of exhaustion, a hacking cough, depression, 15 hours a day in bed most days and many sick visits. Once crying. I googled “ What does it mean when you have high calcium and low Vitamin D. It said 100% of the time it is Parathyroid Disease. I switched Doctors and he believed me and tested me. February 2017 I had my thyroid removed and two glands of my Parthyroid. Now I feel great. If a Doctor discounts you find another one.
Julie,
Thank you for sharing your story and for the important advice. I’m glad you’re feeling so good!
If your calcium is high normal 10 to 10.3, and PTH is also high normal (60) should this be a consideration? Several months ago, after having lots of fatigue and memory loss, I started to wonder if I had sleep apnea. I frequently woke myself snoring, felt like I could sleep at least 12 hours, forgot normal words and where I put things…it was getting bad. Testing revealed only mild apnea, but then I had the blood tests done after my calcium peaked at 10.3 after being stable until last fall at 9.1-9.2. My memory has improved some (nasal strips helped my sleep), but I have painful joints, hair loss, and degenerative disc disease and I feel very old for 46. My NP seems to think all is well, and sent me to a Dermatologist for my hair loss. Any thoughts?
This is an older article so I am not sure if you are still answering quetions, but here goes. I am an active 59 year old, have medical history including hemochromatosis since my 30’s, family history of breast cancer, with my personal history of having very dense breasts with multiple cysts , three biopsies with one showing a radial scar, recent inverted nipple but MRI, mammo, US all look good; chronic neck and musculoskeletal pain. Just recently my dexa scan showed osteoporosis and my labs showed calcium 10.4, normal calcium ionized and normal PTH. CT with contrast showed normal parathyroid and a small 3mm nodule on thyroid. Dr wants me to go on evista for osteoporosis and for lowering my risk for invasive breast CA. I really want to avoid this medication and don’t want to miss if there is something else going on. From everything I have been reading, even though parathyroid hormone levels are normal, there still could be an issue. I do have some of the symptoms including achy joints, fatigue and not resting well, difficulty concentrating. Sure would like to hear your thoughts. Thank you!
I am curious if a high PTH level on its own dangerous. (105.7 then 3 months later, 124) with normal blood calcium (9.6 then 3 months later 9.7) I’ve had a DEXA bone scan (no sign of osteoporosis) and a Sestimibi scan with no adenoma detected. Normal vitamin D levels as well.
I’ve had some symptoms for at least five years now, but not sure if it is the hyperparathyroidism. I’m a 59 year old female. Low (non existant!) libido, GERD, extreme fatigue, anxiety, difficulty concentrating and forgetfulness.
Could the high PTH level on its own cause these symptoms or is it only if the high PTH also causes high calcium levels?
Thank you!
Hi there. I’m so sorry but I’m not a doctor and don’t know the answer to your questions. And I’m sorry you’re having all these issues. Are you seeing an endocrinologist?