My friend Pete, who is in his 70s, had a routine colonoscopy recently. He was relieved when the gastroenterologist told him everything checked out just fine. On the heels of that doctor, though, came another, who announced that Pete had a-fib, which is short for atrial fibrillation. It was discovered because he was under sedation and an anesthesiologist monitored his vital signs, including his heart rate throughout the entire procedure.
Back in January, Pete had another minor procedure that required light anesthesia and vaguely recalls someone saying he had an irregular heart rate, but he wasn’t clearheaded at the time and didn’t give it another thought. This time the message came through loud and clear. He needed to follow up with his doctor.
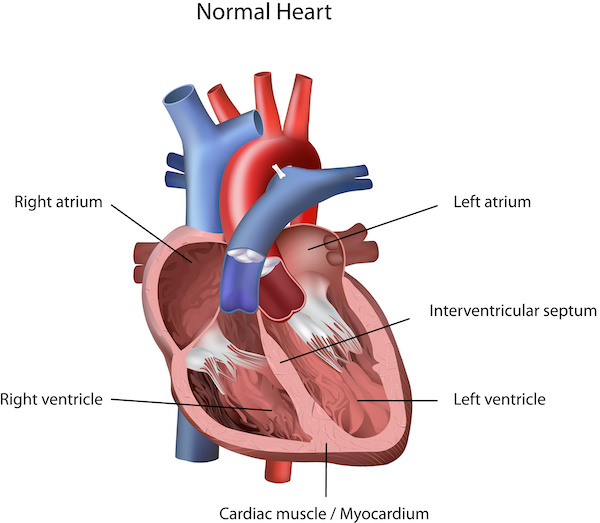

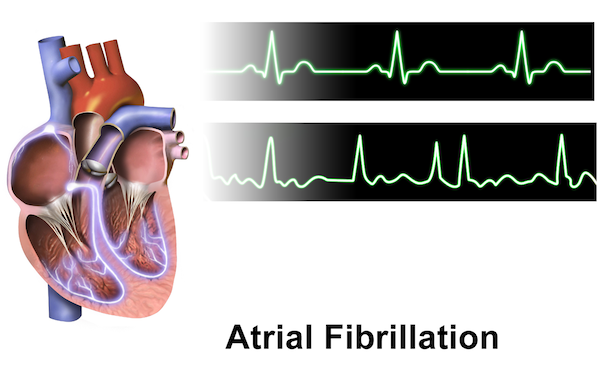
Fibrillation is a problem with the heart’s electrical system, which regulates how fast it should beat and coordinates electrical impulses in the atria and ventricles. When the impulses happen in an organized fashion, it’s considered a normal rhythm. A-fib happens when the impulses in the atria, the top chambers of the heart, are disorganized.
Dr. Andrew Corsello, an internal medicine doctor at MaineHealth who specializes in clinical cardiac electrophysiology, uses “the wave” at a football or soccer game to illustrate the difference between normal rhythm and a-fib.

A good analogy for normal rhythm is when somebody in one corner [of the bleachers] stands up and everyone else in that section stands up after them, and then each person follows the lead of the person next to them. With a-fib everyone is standing and sitting at random. They’re like a bunch of drunks at the game who are not really paying attention to everyone around them.
Andrew Corsello, MD, MaineHealth
You can also have fibrillation in the bottom chambers of the heart — it’s called ventricular fibrillation. That’s a whole different situation, which I will save for another blog post. If you have atrial fibrillation, it can make the bottom chambers irregular and speed up their rhythm, but it doesn’t create the same chaos that would be going on in the top chambers.
When you have chaos in the top chambers of your heart, there are some important things that need to be taken into consideration.
A-fib symptoms
First of all, symptoms. You can have atrial fibrillation and not have any symptoms at all, except maybe you feel a little tired. At the other end of the spectrum you can feel so miserable you rush to the ER.
Pete had no symptoms, except in retrospect he had been feeling a little tired lately.
Absolutely no symptoms, I never felt anything and there are a lot of people who are asymptomatic, evidently. But, then, I know someone who can feel every beat of her heart when it gets a little out of control. The one thing I have noticed, and I don’t know whether it’s because I’m getting a little older, is that I tend to tire a little more easily than I used to.
Pete, a-fib patient
The kind of symptoms someone with a-fib might experience are:
- Palpitations. It feels as if your heart is racing, beating out of sync, or kind of flip-flopping in your chest
- Weakness
- Inability to exercise like you used to
- Fatigue
- Lightheadedness
- Dizziness
- Shortness of breath
- Chest pain
If you’re having symptoms, they may happen only occasionally and last just a few minutes or occur frequently and go on for weeks. In some cases, they persist even longer or may not go away on their own at all.
A-fib and heart failure
Second, it’s not the norm, but Dr. Corsello says in a subset of patients, a-fib can weaken heart function and result in heart failure, which means your heart can’t circulate the amount of blood your body needs to function properly. “That’s why you have to be diligent about figuring out what is going on and be aggressive about treatment,” says Dr. Corsello
Important tests
Some common tests when a-fib is suspected include:
- Electrocardiogram (ECG, EKG). A primary test for diagnosing atrial fibrillation.
- Holter monitor. A portable ECG device that records your heart’s activity over a 24-hour period.
- Event recorder. Another portable ECG device that monitors heart activity over a few weeks or months. If you experience symptoms, you push a button, and heart activity is recorded for a few minutes.
- Echocardiogram. A test that uses sound waves to create moving pictures of the heart. It is used to diagnose structural heart disease or blood clots in the heart.
- Blood tests to rule out health conditions that might lead to a-fib, such as thyroid issues.
- Stress test. While you are exercising (usually on a treadmill) various tests are run on your heart.
- Chest x-ray. Images of your lungs and heart, which may rule out or uncover other issues or conditions.
By BruceBlaus – Own work, CC BY-SA 4.0, Wikimedia Commons
What causes a-fib?
A-fib can be caused by a number of things, most commonly abnormalities or damage to the heart. Other possible causes are:
- High blood pressure
- Heart disease (valve problems, congenital heart disease, congestive heart failure, coronary heart disease, history of heart attack or heart surgery
- Thyroid disease, usually hyper (overactive) thyroidism
- Medications, caffeine, tobacco, or alcohol
- Lung diseases
- Virus
- Previous heart surgery
- Sleep apnea
- Stress related to surgery or illness
- Age. Risk increases with age
- Family history
- Obesity
Pete had most or all of the recommended tests, which confirmed he had a-fib but found no other issues. His age may play a role, and he was diagnosed previously with high blood pressure but says it is now normal with medication. He thinks his a-fib may have been triggered when he had had his recent medical procedures.
A-fib and the risk of stroke
The third thing Dr. Corsello says needs to be considered when someone is diagnosed with a-fib is that it increases the risk of stroke. What happens is the irregular rhythm can cause blood to pool in the atria and form clots, which can dislodge from your heart and travel to your brain. If a clot gets stuck in a blood vessel it can block the flow of blood to the brain and cause a stroke.
That’s the one thing that we really fear and sometimes concentrate on in patients without symptoms because your risk of stroke goes up probably about five-fold once you have been diagnosed. That risk is nearly brought back to normal if a person who qualifies for it takes a blood thinner. It takes some testing and time to tease out which subgroup a patient fits into. Every single patient is different.
Dr. Corsello
Your risk of stroke increases if on top of having a-fib, you are older and have other stroke risk factors such as high blood pressure, diabetes, a history of heart failure, or a previous stroke.
Overall, Pete’s health is good. While he doesn’t have a lot of stroke risk factors, he has some, so, to reduce his risk, Pete’s doctor prescribed a blood thinner.
I am now taking Eliquis, a blood thinner, plus amlodipine, a blood pressure drug. My cardiologist said this is safe and necessary in case a fib returns.
He also opted for a treatment called electric cardioversion to restore his heart rhythm to normal.
They put a small patch on your back and one on your front. They’re maybe an eighth of an inch thick and not like the paddles they use trying to bring somebody’s heart back. It’s a shock to your heart that resets the rhythm and it only takes one second. They put you under a mild sedative for a very, very short period of time and then they monitor you for an hour afterwards to see if your AFib is still there. Mine disappeared and a few days out it’s still gone. I also bought a cool little monitor that does an EKG and checks for an irregular hearbeat.
Pete
Cardioversion can also be done with drugs called antiarrhythmics. The use of either form of cardioversion depends on the underlying cause of the a-fib and how long it has been happening.
A medication such as a beta-blocker, which slows the heart rate might also be prescribed. If nothing else works to control the a-fib, it may be necessary to try an ablation procedure, such as a radiofrequency ablation, which destroys the heart tissue that is causing the problem.
Treatment goals
Resetting the heart rate to a normal rhythm and preventing stroke are the two primary treatment goals for a-fib. As Dr. Corsello mentioned, each patient is different. In some cases, he says the appropriate treatment approach may be to watch and wait. In others, it’s to prescribe a blood thinner, which can help prevent blood clots from forming. The downsides, depending on which blood thinner you’re on, are that it can be inconvenient if routine blood tests are necessary, there’s an increased risk of bleeding, and it can be expensive.
What you do first is look at the risk of the patient having a stroke, period, and then, if they also have a-fib. That’s how you decide whether the risk of a blood thinner is justified.
Dr. Corsello
A rising problem
Dr. Corsello says a-fib is getting more and more common. 2.7 million Americans and counting. Why so many?
We think people are living longer with their heart disease. Number two, and this is depressing, the U.S is getting more obese. Each kilogram you gain has a statistical increase in your percent of a-fib. Some of it is because of sleep apnea. Once people get big enough, sleep apnea becomes common. Some of it may be through high blood pressure, diabetes, and other things that certainly increase the stroke rate, but some of it is directly related to obesity. I see a lot of shocked faces when people ask why am I having a-fib and I say, well, because of your weight. Obesity is a major, major risk factor for a-fib and everything that goes along with it.
Dr. Corsello
You may not always be able to prevent a-fib, but switching to a healthier lifestyle could give you an edge against it and all sorts of other diseases and health conditions. To begin with, don’t smoke, follow a heart-healthy diet, be physically active, and cut back on alcohol. Does the thought of any of those suggestions make you groan? Consider the possible alternative.
In Pete’s case, he doesn’t smoke and eats a fairly healthy diet, but he really enjoys a shot or two of good bourbon. His doctor suggested he save bourbon for special occasions. Pete’s giving it careful consideration.
Bottom line: if you suspect you might have an irregular heart rate or if you have any risk factors, take it seriously and see your health care provider.

Diane, this is a great article. My husband just went through heart surgery and had many of the symptoms but no one put all of them together to really understand his condition(s). He had surgery in January for a blocked artery. After surgery he went into congestive heart failure and would have died if we had not rushed him back to the hospital. He has recovered and has more energy than at anytime during the last 20 years!
I am so glad they figured it out and that he’s doing better! A happy ending story.
Diane, Thank you for the very clear treatise on the description, causes and remedies for a-fib. I’ve had it for a very long time and, in reading your column, I could check off all the things I’m during right to treat/control it. Thank you. John T.
Hi, John! You are welcome and it’s great to hear from you