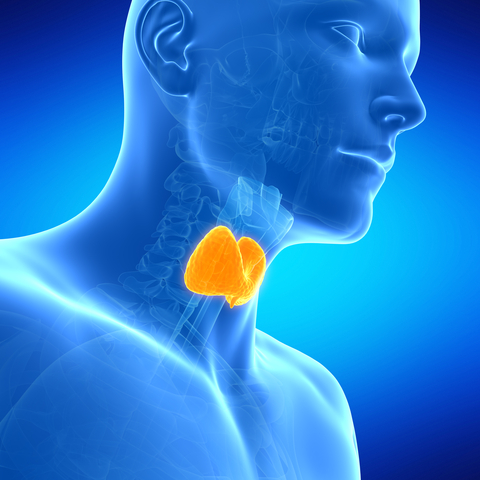
Thyroid trouble? As we age, the risk of our thyroid not working properly increases. I know, yet another thing. The thyroid gland is a butterfly-shaped organ in the neck, just above your collar bone and below your voice box. If you’re a man, it’s not your Adam’s apple, it’s just below it. The thyroid’s job is to produce hormones that regulate how the body uses and stores energy. It can be under- or overactive. It can develop lumps or nodules. Or it could become cancerous.
According to the American Cancer Society, in 2016, there will be an estimated
- 62,450 new cases of thyroid cancer in the United States (49, 350 in women and 19, 950 in men)
- 1,980 thyroid cancer deaths (1,070 women and 910 men)
- The death rate has been fairly steady for many years and is low compared with most other cancers
There are four general types of thyroid cancer. Most cases are very curable.
- Papillary
- Most common (About 80%)
- Follicular
- Medullary
- Anaplastic
One type of thyroid cancer gets a new name
Recently, a panel of doctors from around the world reclassified and changed the name of a type of papillary thyroid cancer. Encapsulated follicular variant of papillary carcinoma or EFVPTC is now noninvasive follicular thyroid neoplasm with papillary-like nuclear features or NIFTP. Simply put, they’re not calling it cancer anymore.
Why the change? An independent team of pathologists reviewed 268 tumor samples. The patients had all been diagnosed with EFVPTC, which, again, is a variant of the most common type of thyroid cancer — papillary cancer. Some had an invasive form of the disease, meaning it had spread and some had a noninvasive form meaning it had not spread.
They decided to make the change because their study concluded that “Thyroid tumors currently diagnosed as noninvasive EFVPTC have a very low risk of adverse outcome.” In other words, they generally don’t do anything. They just stay put and don’t spread. You’ll find the details of the study in an online article published April 14 in JAMA Oncology.
How might this change make a difference for someone? It could mean less surgery and no cancer treatments. You need surgery to get an accurate diagnosis in the first place, but the usual course of action when someone is diagnosed with EFVPTC is to treat it as if it were cancer. “It makes people less likely to have future unnecessary treatments, such as radioactive iodine or possibly a second surgery to completely take out the other side,” says Dr. Christine Twining, MD. She is the Medical Director of Maine Medical Partners Center for Endocrinology and Diabetes. Dr. Twining did not participate in the study, but one of her specialties is thyroid diseases, including cancer. She goes on to say “For example if someone only had half of their thyroid removed and a cancer is found, some surgeons would automatically remove the other side. Because of this reclassification, you might not take the other side.”
Increased thyroid cancer rates
Another important change is that in the last 30 years or so the rate of thyroid cancer, particularly small growths, has increased dramatically. A study reported in JAMA in April 2014 looked at the increased rates. The authors found that “Since 1975, the incidence of thyroid cancer has now nearly tripled, from 4.9 to 14.3 per 100, 000 individuals.” They concluded that rather than an “epidemic of disease” it was actually an “epidemic of diagnosis.”
“I think some of it is from an increase in detection,” says Dr. Twining, who was not involved in the study. “We have much more accessible imaging, so people are having more imaging tests than they used to. Thyroid nodules are getting picked up by carotid ultrasounds,
[Tweet “The majority of thyroid nodules are not cancer.”]
Thyroid nodules
A few years ago, I wrote about my friend Lee. A CT scan for something else picked up a small nodule on her thyroid. A fine needle aspiration biopsy came back suspicious for papillary cancer. She had surgery, which, thankfully, confirmed that the nodule was benign.
Thyroid nodules are very common as we get older. “By the time we’re 50, 50 percent of individuals will have a thyroid nodule, ” says Dr. Twining, “and that goes up linearly pretty much with age. If you look at incidence rates, 70 percent of 70-year-olds and 90 percent of 90-year-olds will have nodules. Most of them are not cancer. If you look at studies, on average, maybe five percent are cancer.”
The best way to detect thyroid nodules is with ultrasound, but most doctors don’t recommend using ultrasound to simply screen for nodules. “Anyone who has a palpable nodule should certainly have an ultrasound or if there’s a symptom that might indicate there’s a thyroid nodule — those might be triggers to get an ultrasound,” says Dr. Twining. “But if we were screening everybody, we would pick up lots of people who didn’t have a problem at all who didn’t need to worry. Most of them are not [cancer].”
Thyroid cancer symptoms and risk factors
Oftentimes, there are no signs or symptoms, but here are some that you should pay attention to:
- Lump in the front of the neck, just below the Adam’s apple or where it would be if you had one (women)
- Swollen lymph nodes in the neck
- Hoarseness
- Difficulty swallowing or breathing
- Throat or neck pain
Here’s what may increase your risk:
- History of radiation exposure to the head and neck
- Family history of thyroid cancer
- Age under 14 or over 70
- Being a man
- A diet low in iodine
Most of the time, thyroid cancers are picked up because someone feels a lump in the neck or his/her provider notices something during a routine check up. (Your doctor should always do a neck check when you have a physical.) And, as we’ve seen, they get picked up by chance. Fortunately, most thyroid cancers can be successfully treated with surgery and radioactive iodine treatments.
As for the recent name change, just removing the word cancer should ease some people’s mind. There are similar discussions about some other cancers, including DCIS, which I was diagnosed with two years ago.
But the reclassification also presents some new challenges for physicians. At the time I interviewed Dr. Twining, the JAMA article had been published only a few weeks earlier. “And it was a fairly small sample size,” she says, “so we don’t know as a medical community exactly how we’re going to process and use that information.”
The important thing is that if you have any concerns, make sure to get them checked out. And be ready with the questions you want to ask. If you’re not sure what to ask, here are some good pointers to get you started. If you have already been diagnosed with thyroid cancer, Dr. Twining recommends thyca.org as a good source of reliable information.
This post was originally published on the Advantage Home Care blog, which I also write.

Leave A Comment