Guest post by Chelsea Ginn, FNP-BC
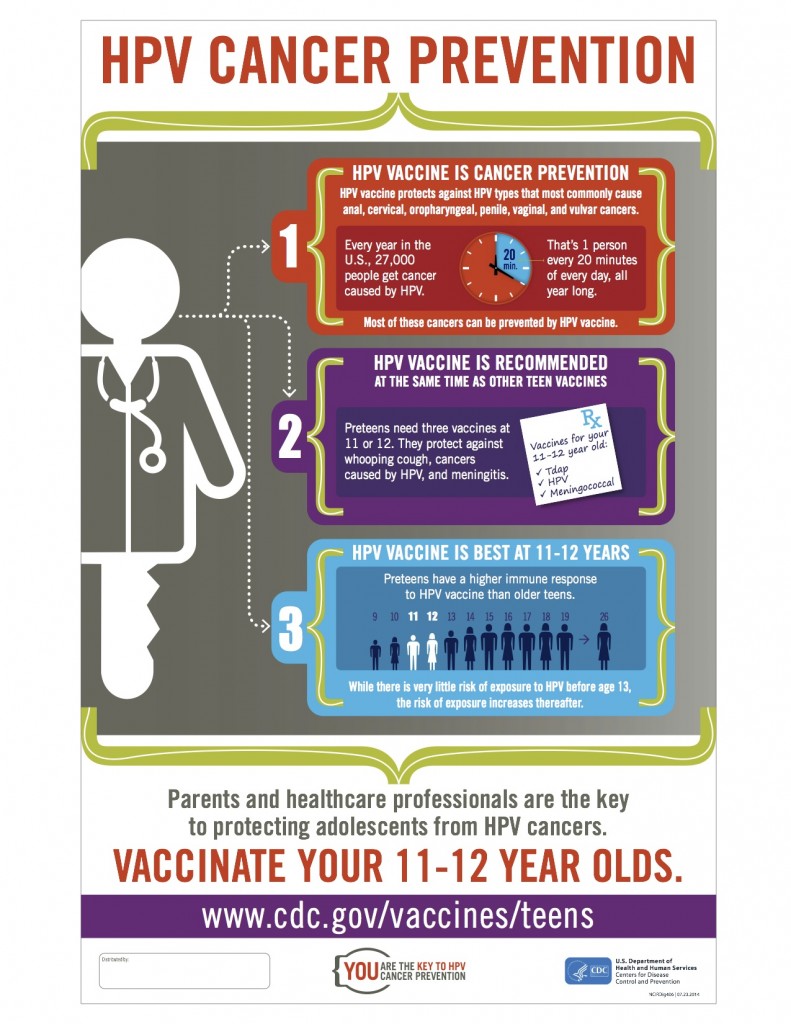
Cervical cancer is caused by a virus known as the human papillomavirus (HPV). Not only is it one of the few types of cancer for which the cause is known, but it’s also one of only two types of cancer that can be prevented with a vaccine.
That’s good news because HPV is extremely common. It’s estimated that 80 percent of people will get the virus at some point in their lives though most will never know they’ve been infected. When the infection doesn’t clear on its own, HPV can lead to genital warts or certain cancers. This includes cervical, vaginal, and vulvar cancers in women, penile cancer in men, as well as anal cancer, and mouth/throat (oropharyngeal) cancer in both men and women.
In the United States alone, 27,000 people are diagnosed with an HPV-related cancer every year. 27,000 translates to a new case every 20 minutes!
How do we get exposed to HPV?
HPV is primarily spread during vaginal, anal, or oral sex, but a person doesn’t need to have sexual intercourse to get infected. Since HPV is spread through skin-to-skin contact, the virus can enter your body through a cut, scrape or small tear in the outer layer of your skin. HPV can be passed even when an infected person has no signs or symptoms.
How is HPV diagnosed? What screenings exist for cervical cancer?
HPV infections often don’t have warning signs or symptoms. For many years, women had to rely on annual Pap tests (the legs in the stirrups image come to mind!?) to identify abnormal changes in their cervical cells, which can happen as a result of HPV infection, but also other infections.
So, unfortunately, a Pap test is not the most effective way to diagnose an HPV infection because it simply tells women and their healthcare provider that there are such changes, but not the cause. Therefore, women may have to undergo further testing to determine the cause of the infection and then invasive procedures to treat it. And even then, about 15 percent of women with pre-cancerous cell changes are missed through these screenings.
More recently, an HPV test has been developed that looks for the types of HPV most likely to cause cervical cancer. The test is done very similarly to a Pap test and can often be done at the same time as the Pap test. Once again though, it is not a preventative screening, but a test that identifies when a woman has already been infected with HPV.
This is why, despite screenings and treatment, roughly 12,000 women are diagnosed with cervical cancer and 4,000 women die each year in the U.S. alone.
How can we prevent HPV infections?
Through a safe and effective vaccine!!
The most commonly used HPV vaccine protects against four strains of the virus, including two of the most common strains (16 and 18), which are responsible for 70% of cervical cancers and 90% of genital warts.
And there is more good news on the horizon. A new HPV vaccine has been approved that protects against five additional strains. Data from the extensive clinical trials of this new HPV vaccine, called the nine-valent vaccine, show that it can protect against 9 different HPV strains and prevent approximately 90 percent of invasive cervical cancer cases worldwide.
In December 2014, the FDA approved this new HPV vaccine, and next month, the Advisory Committee on Immunization Practices (ACIP) will meet to discuss formal recommendations for the nine-valent HPV vaccine.
When can people get vaccinated against HPV?
The current HPV vaccine is given in a series of three shots. It is recommended for both boys and girls beginning at age 11. Vaccinating against HPV at this age helps make sure that children and teens are protected before they are exposed. Even if tweens and teens are not having sexual intercourse at this age, they may be experimenting with the other behaviors that could lead to exposure.
Because HPV is so common and doesn’t always have symptoms, no one can predict if a potential sexual partner is infected or not (unless he or she was tested previously). It’s important to know that the vaccine can be administered up to age 26 so that even if someone has already been sexually active, they can still be protected from further infection going forward.
We want to encourage people to learn more about HPV and cervical cancer prevention and to get vaccinated against HPV if they haven’t already!
Take a moment to look at the resources below and learn more – for yourself, your loved ones, and your community.
- Like the Vax Maine Kids Facebook page or follow @VaxMaineKids on Twitter to receive updates regarding the new HPV vaccine.
- Visit the CDC website to learn more about HPV vaccination.
- Support The Yellow Umbrella Organization and hear how cervical cancer survivor Christine Baze is using her musical talents to help educate people about cervical health and to encourage them to get vaccinated and screened.
- Listen to as many as 20 different personal stories of those who have been impacted by HPV and cervical cancer on the Shot By Shot.
- Check out this powerful new documentary Someone You Love: The HPV Epidemic and visit hpvepidemic.com to learn more about attending a screening or holding one of your own.
For more information on the importance of all childhood immunizations, visit Vax Maine Kids.
This post was written by Chelsea Ginn, FNP-BC, a board-certified family nurse practitioner at Maine Medical Partners Westbrook Internal Medicine. Chelsea provides comprehensive primary care with a focus on prevention, chronic disease management and women’s health issues.


Leave A Comment