The challenge of treating cancer
Cancer. Such a formidable word. The big C, as some people call it. Finding a cure for cancer has been difficult — more so even than finding one for HIV, says medical oncologist Dr. Peter Rubin. “People spent the time to figure out what was driving HIV,” he says. “Unfortunately, cancers are tremendously more complicated than HIV.”
Dr. Rubin is the Medical Director for Southern Maine Health Care’s Cancer Care and Blood Disorders practices. He says finding a cure for cancer is such a challenge because not all cancers are the same. What drives one cancer to grow and spread does not necessarily drive another.
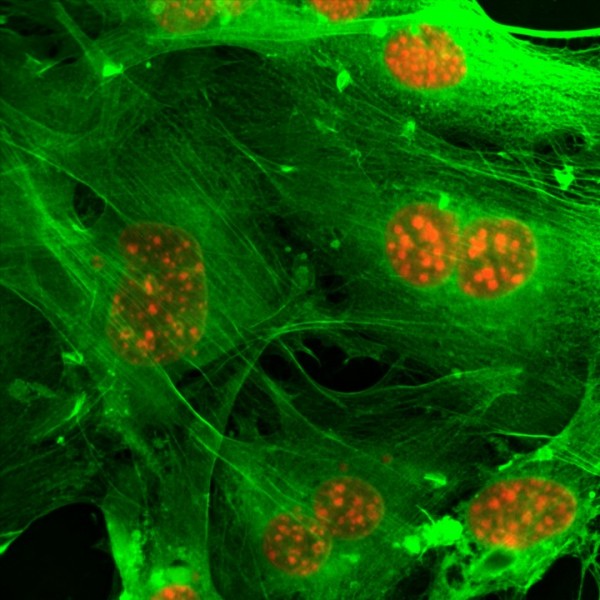
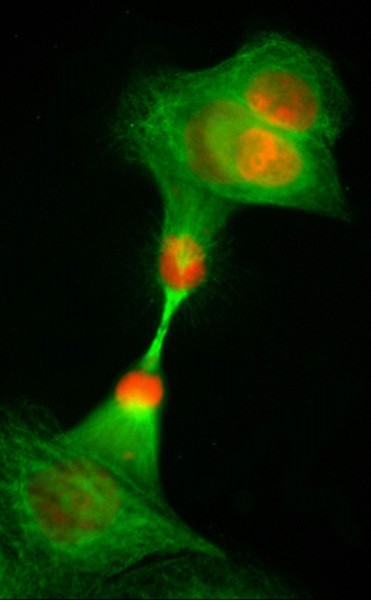
Cancer happens when cells divide and multiply at an abnormal rate. Normal cells know when to stop dividing. Cancer cells don’t. Normal cells also know when to die. Cancer cells don’t.
What makes it happen? According to the American Cancer Society, “Cancer can arise from any number of genetic malfunctions, and often is due to a combination of errors.”
The most critical feature of cancer cells is that they can spread or metastasize. “If you had a cancer that was growing in one place, you could cut it out,” explains Dr. Rubin. “It may grow back, but you could do radiation. If cancer didn’t spread we would not have the problems we have. When it spreads or disseminates throughout the body, it’s just that much more difficult to get rid of it. That’s the whole other aspect of treatment. How do you prevent metastasis? How do you prevent cancer from spreading?”
Not too long ago, the only effective treatments were surgery, radiation therapy, and chemotherapy. Today, targeted therapies and immunotherapy have become an important part of the mix.
Targeted therapies
You may have seen ads on TV for various cancer drugs. Drugs that you might think are chemotherapy drugs, only they seem different. They are different — they’re targeted therapies.
“Chemotherapy is like shooting the howitzer and trying to destroy as much of the enemy as possible,” says Dr. Rubin. “Targeted therapy is more selective and very discrete and delicate. You’re trying to disable a cancer by understanding something about it. You’re targeting the most critical part of the engine that is driving it.”
There are two types of targeted therapies: monoclonal antibodies and small molecule drugs. Their targets are the mutated genes that are causing the cancer to spread. There’s a difference in how the cancer cells respond to these targeted therapies. “You’re actually disabling the cancer cell in a different way but not necessarily killing it,” says Dr. Rubin. You may be putting it in some resting state, preventing it from growing.”
The challenge with targeted therapies is figuring out the mechanism that drives a particular person’s cancer. Not all tumors have the same target so a drug may work for one person, but not another. “Mrs. Jones’ breast cancer is not going to be the same as Mrs. Smith’s,” explains Dr. Rubin. “She may have a mutation that’s different — that we can use a particular drug on.”
Right now, some of the more common targeted therapies are being used to treat lung, breast, and colorectal cancers and malignant melanoma. Research is ongoing, including into targeted therapies that can be used to treat more than one cancer.
There is a genetic mutation linked to some lung cancers, for instance, that can be treated with a targeted therapy. If the same genetic mutation is found in another cancer, such as colon cancer, Dr. Rubin says there’s a good chance the lung cancer drug would also work with colon cancer. Again, it’s all about targeting whatever mechanism is driving the cancer cells.
Immunotherapy
Immunotherapy is another new and promising cancer treatment. Drugs called immune checkpoint inhibitors are used to target the immune system.
Our immune system has the ability to detect and destroy cancer-causing cells. Unfortunately, sometimes it doesn’t work as it should. We also now know that the cancer itself can prevent the immune system from generating a response.
Immunotherapy drugs reactivate or strengthen the immune system and, in theory, destroy the cancer cells. “A couple of drugs have been extraordinarily potent in terms of their ability to not only destroy one type of cancer but multiple types, lung, pancreas, and brain for example — just a huge number of these cancers. Before we would have had one regimen that was specific for one type of cancer. Now we have these immune checkpoint inhibitors that seem to target the immune system regardless of the cancer for the most part.”
As with targeted therapies, immunotherapy research is ongoing. For example, scientists are looking at how combining immunotherapy with other types of cancer treatment may boost its effectiveness.
Personalized cancer treatments
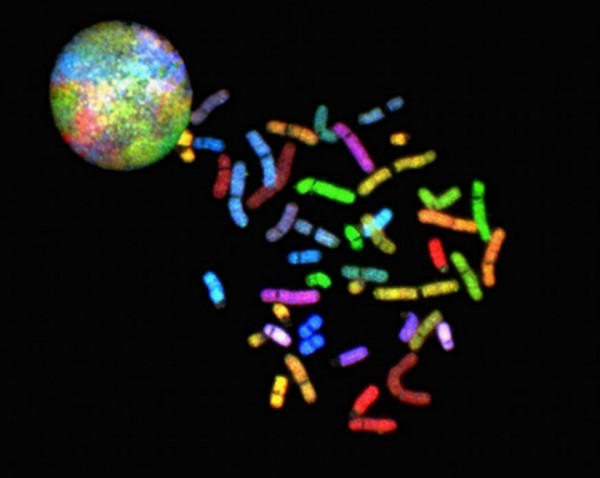
Eventually, when someone is diagnosed with cancer, the treatment will be personalized according to whatever genetic mutation is driving the cells to grow and spread. “For example,” says Dr. Rubin,” when people get diagnosed with cancer, Dana Farber, which we’re now collaborating with, takes their tumor and looks for the 300 most common mutations that you see in cancer. Let’s screen people for all these mutations on the off chance that if they do have a mutation a particular drug may be effective. This approach is called oncogenomics or personalized oncogenomics.”
In layman’s terms, it’s known as personalized cancer treatment. Being able to treat an individual based on the genetic makeup of his/her cancer cells. To target those cells with a specific drug that will work and without the usual debilitating side effects.

Leave A Comment