Clayton’s story
A few years ago, Clayton Douglass went to his local quick care clinic to have a rash under his arm checked out. The doctor didn’t know what it was and prescribed a cream, which didn’t work. The rash spread. Clayton spends a lot of time in the woods, so suspected he might have Lyme disease.
“I’m constantly dealing with ticks,” he says. “I looked it up on the Internet and found pictures that looked exactly like what I had. I went back to the doctor, showed him the rash again and suggested that it might be Lyme disease. He looked it up in a medical journal and agreed. He then put me on a 21-day treatment of doxycycline. The rash cleared up and I haven’t had any problem since. I was lucky. Many people don’t get treatment until it’s too late. Ticks are an epidemic. A vaccine would be nice …”
Jennifer’s story
When Jennifer MacFarland’s son was three years old, she noticed the left side of his face had a slight droop. “When we called the pediatrician,” she explains,” he told us it was due to seasonal allergies — that the tissue in the face “swells” and contracts the nerves. Within two hours our son was violently vomiting clear thick liquid. We brought him to the ER. They ran tests for hours. Finally, they decided to do a spinal tap. The results showed he had Lyme meningitis, which explained why his face drooped. He was under the direct care of the CDC for three months at The Barbara Bush Children’s Hospital. He’s a healthy boy now, but his immune system hasn’t been the same. A common cough that should last four to seven days takes three to four weeks to run its course. I think ticks and Lyme disease education is super important!
Justin’s story
Jennifer’s son’s drooping face was a sign of Bell’s Palsy, rare in children, but something that can occur with Lyme disease. It happened to my nephew Justin Cross, who works in the woods and is super diligent about checking for ticks. A few years ago, he found a deer tick in his mustache — attached, but not engorged. No rash appeared, so he didn’t worry. Several weeks later his joints began to ache and then he lost his sense of taste. “My taste buds went on Wednesday,” he says, “and then on Friday I was at work and tried to whistle a tune, but couldn’t. I found a mirror and the whole left side of my face was just hanging!”
Deer ticks — tiny creatures that barely tickle when they crawl over your skin. Makes me shudder just to write the sentence. If you hoped they didn’t survive the winter, forget that notion. They did and already, more than 50 cases of Lyme disease have been reported in Maine. Last year, more than 1,375 cases were reported, which was a record high for the state.
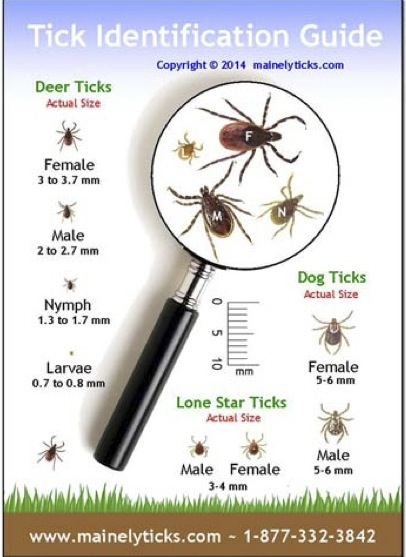
Not all ticks are deer ticks. Did you know that in Maine alone, 14 different tick species have been identified? Thankfully, they don’t all feast on humans. Only one, the deer tick, is responsible for most of the tick-borne illnesses in humans in this state, primarily Lyme disease. If a tick is making a meal of you, determining if it’s a deer tick is important. This guide from Mainely Ticks is helpful because it shows actual tick sizes.
According to the Maine Medical Center Research Institute, about two-thirds of the cases of Lyme disease in Maine are reported in June, July, and August. That’s because the peak season for deer tick nymphs is June and July. All stages will bite humans, but because the nymphs are tiny and their bite painless, they often get missed.
Always check yourself, your children and your pets thoroughly after being outdoors. Something I just found out: Lyme disease is most common among school-age children and adults over 65.
If you find a tick, the sooner you remove it, the less likely you’ll get a tick-borne illness. Not all deer ticks carry Lyme disease, but better safe than sorry. The University of Maine Cooperative Extension Tick Id Lab states that although in Maine Lyme disease is the number one infection to be concerned about, deer ticks can also transmit anaplasmosis, babesiosis, and Powassan virus.
How to remove a tick
Using tweezers
- Grasp the tick close to the skin with fine-tipped tweezers.
- Pull gently upward with steady, even pressure until the tick lets go.
- Try not to squeeze, crush or puncture the body of the tick, because its bodily fluids may contain infection-causing organisms.
- After removing, thoroughly clean the bite area and your hands with rubbing alcohol or soap and water.
- Don’t use Vaseline, alcohol or nail polisher remover because they don’t work.
- Save the tick in a small bottle in case it needs to be identified. Mark it with the date and where it was attached.
-
Consult a physician if you removed an engorged tick or if you develop a rash or fever within several weeks of removing the tick.
Using a tick removal spoon
- Put the notch on the spoon on the skin near the tick.
- Apply downward press and slide spoon forward to frame the tick. Keep sliding spoon forward to detach the tick.
- After removing, follow same steps as above.
If you find any ticks on you, try not to freak out, but again, do remove them promptly. To have a tick identified, for $10.00 you can mail the specimen or upload a picture of it to the Tick Id Lab in Orono. In most cases, a deer tick needs to be attached for 24 to 48 hours before it can transmit Lyme disease. To be on the safe side, you should be on the lookout for any symptoms, which usually show up from 3 to 30 days after a bite.
Lyme disease symptoms
Stage 1 symptoms of Lyme disease (usually occur within a month)
- Chills
- Fever
- Headache
- Lack of energy
- Achy joints or muscles
- Rash that resembles a bull’s-eye (an estimated 70% to 85% will get a rash)
Stage 2 symptoms of Lyme disease (one to four months)
- Tiredness
- Additional rashes
- Pain, weakness or numbness in the arms or legs
- Paralysis of nerves in the face
- Recurring headaches or fainting
- Poor memory, inability to concentrate
- Conjunctivitis
- Occasional rapid heartbeats
Stage 3 symptoms of Lyme Disease (several months or years)
- Joint swelling, especially the knees
- Numbness and tingling in hands, feet or back
- Severe fatigue
- Neurologic changes
- Chronic Lyme arthritis
Lyme disease is easily treated in the early stages with antibiotics, which are also used to treat later stages of the disease. There used to be a vaccine available, but it was taken off the market in 2002, supposedly because there wasn’t enough demand.
Testing for Lyme disease
Some individuals, including Bob Maurais, believe that you shouldn’t wait if you suspect a tick-borne infection. “If you remove and positively identify the tick as a deer tick, seek out a physician who will begin antibiotics,” he urges. “Don’t wait for the results of blood work that is oftentimes not accurate.”
That’s what happened to Michael Anderson. In 2008, he saw his doctor because he thought he had the flu. Then one night his lower back felt itchy and when he looked in the mirror he saw a round rash circling a deer tick. “I went back to my doctor and he didn’t really think it was Lyme disease. He ran the local lab Lyme test, which was negative. So I took his word.”
Michael was eventually treated but now has chronic Lyme disease. You can read more about his story in my blog post, One Man’s Ongoing Struggle with Lyme Disease.
I don’t know exactly what blood test Michael had initially, but the CDC currently recommends a two-step process when testing blood for evidence of Lyme disease antibodies.
- The first step uses a testing procedure called “EIA” (enzyme immunoassay) or rarely, an “IFA” (indirect immunofluorescence assay).
- If this first step is negative, no further testing of the specimen is recommended.
- If the first step is positive or indeterminate (sometimes called “equivocal”), the second step should be performed.
- The second step uses a test called an immunoblot test, commonly, a “Western blot” test.
Results are considered positive only if the EIA/IFA and the immunoblot are both positive. The two steps of Lyme disease testing are designed to be done together. CDC does not recommend skipping the first test and just doing the Western blot. Doing so will increase the frequency of false positive results and may lead to misdiagnosis and improper treatment.
Tick emergency preparedness
In the words of Ben Franklin, “An ounce of prevention is worth a pound of cure.” That includes trying to protect yourself against ticks in the first place.
- Try to avoid known tick-infested areas and if you can’t, plan activities for hottest, driest part of the day.
- Wear light-colored clothing.
- Wear long pants tucked into socks or boots and tuck shirt into pants.
- Don’t wear open-toed shoes or sandals in areas that may harbor ticks.
- Consider using a tick repellent. For more information, read this insect repellent fact sheet.
- Check yourself over carefully after you’ve been outdoors and make sure to look under your arms, behind the knees, between the legs, in and around the ears, in the belly button and in the hair.
Bob Maurais points out that you don’t have to be hiking the Appalachian Trail to come head to head with a deer tick. Most likely it’ll happen right in your own backyard. “It’s estimated that 75 percent of Lyme disease cases are contracted within 100 feet of the house,” he says.
Clayton Douglass says he hasn’t found anything yet that does a good job of repelling ticks. “I do use DEET,” he says, “but I think it only cuts down on the numbers of them I find. A couple of years ago I went deer hunting off the Webb Road in Windham. When I got back to my truck, I started picking off little black deer ticks. I counted over thirty of them! I’ve heard people say that part of the problem is people don’t burn their fields like they used to 40-50 years ago. I don’t know the answer. DDT used to kill a lot of them, but I’m still glad they stopped spraying that stuff around. I see a lot of eagles now. I’ll deal with the ticks to enjoy that sight!”
Do you have any advice to share?
Have you found a way to protect yourself against ticks or have you had experienced Lyme disease and have some important information to share? Add your comments below or send me a personal message and I’ll do a follow-up blog post. Thank you!




My Dog just passed away. Our vet told us that it was due to Lyme Disease, please peruse this document and ensure that your dog is treated
Lyme Disease revisited? The first time I got it, 2 years ago, my rash was unlike anything either my doctor or dermatologist had seen. Both gave me lyme disease tests. The initial test was positive. She wanted to wait another week plus for the Western Blot disease results before taking action, but my joints were so swollen I couldn’t find my ankles. So she started the 4 weeks worth of antibiotics right away. Eventually all the tests came back and were all positive. 4 weeks sounds like a long time, but if your doctor is prescribing less than 3 weeks – it’s time to shop for a doctor who knows what s/he is doing – you could be in serious trouble in the long run by taking too few antibiotics for this nasty disease.
What was upsetting was the cost of the Western Blot test. On most insurance policies, lab tests are billed as first dollar until deductibles are met (while other visits are billed at the co-pay or 20%). So if this is one of your first doctor visits of the year, expect bills of well over $500 for the Western Blot test from many labs.
We need legislation requiring medical costs to be posted online, including the percentage discounted for medical plans. Not complicated for a decent programmer and organized billing department.
This time many of the same symptoms are present. Avoiding ticks are nearly impossible in our environment, although I’ve tried taking the precautions. The doctor I saw today is putting me on antibiotics without the Western Blot test, which may be positive (anyway) because of the prior incident. It took the medical lab over 20 minutes to get the price of the blood tests from the only lab they use because of recorded menu selections, being put on hold, and plain disorganization. 20 minutes.
There are labs that charge less than half of what our local hospital (which owns the clinic I’ve gone to for the last 20 years) charges. Patients are starting to shop for better pricing. Do your homework if you don’t have cash to throw out–Head’s up!