More than 40 years in retail — standing for hours on end several days a week — took its toll on Jane Smith’s legs. Both had bulging, ropy varicose veins running down them, one from thigh to ankle. “These were not small spider veins,” says Jane. “These were big. I used to be embarrassed and always wore pants to hide them.”
Used to.
Today, Jane’s legs not only look better, but they also feel better. Relief came at the hands of Dr. Cindy Asbjornsen, a board-certified family practice physician and a board-certified phlebologist or vein specialist. In the “old days” a common treatment for people with varicose veins like Jane’s was to strip the vein — surgically remove it. It’s still being done, but generally, only with very large veins. Instead, the standard of care is minimally invasive techniques, which can usually be done with a local anesthetic right in the office. Dr. Asbjornsen used two treatments on Jane — ultrasound-guided sclerotherapy and endovenous laser ablation.
A key to successful treatment, said Dr. Asbjornsen, is locating the source of the problem. An important search tool is ultrasound. “Ultrasound has changed dramatically in the last 20 years and now it can show quite literally what direction blood is flowing in a vessel,” she explained. “If you stand up, blood in the arteries should flow toward the feet and veins should be carrying blood back up to your heart. If I see it going in the wrong direction, it’s a problem.”
The problem is usually that a valve has stopped working somewhere, preventing blood from returning to the heart. Instead, it flows back down into the legs and pools. The goal is to plug the leak or leaks, which usually takes a series of treatments or combination of treatments. “If you treat the source of the problem,” she said, “your body will just take care of what’s left over. It’s important to realize, though, that you’re not going to wake up the next day with beautiful legs. A lot of times it’s a solid six months after treatment.”
Treatments for vein problems
- Sclerotherapy treats tiny veins just below the skin’s surface. Using a small needle, a substance is injected into the vein, which makes it become sticky. It then seals shut and disappears.
- Light-assisted sclerotherapy also treats hard to see veins below the skin’s surface. A small hand-held light illuminates the veins and makes them easier to see.
- Ultrasound-guided sclerotherapy uses ultrasound to locate veins. It is often used to treat veins that connect superficial veins that lie above leg muscles to deeper veins that lie under and between leg muscles.
- Ambulatory phlebectomy treats small varicose veins that are too big to be treated with sclerotherapy. It is a minimally invasive procedure that involves removing the vein through tiny incisions in the skin. It is done under local anesthesia and in most cases, stitches aren’t needed because the incisions are so tiny.
- Endovenous laser ablation has become the gold standard in the treatment of large varicose veins. A small laser fiber is threaded into the vein. The laser heats the lining of the vein, which makes it collapse, shrink, and disappear. The procedure is done in the office and takes about 30 minutes.
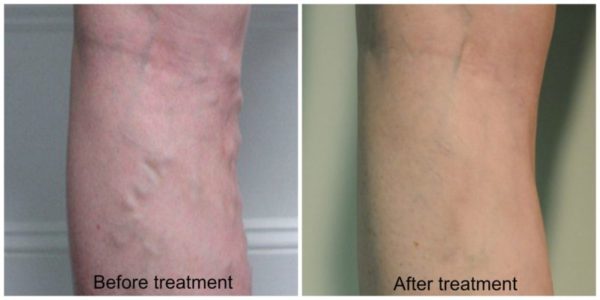
Before and after pictures
Common symptoms
Some people with vein problems may not realize it because they don’t have ropy veins on the outside of their leg like Jane and symptoms can be subtle. A telltale sign is if you wake up feeling fine, but by mid afternoon your legs feel heavy, achy, or tired. You might also notice that your shoes feel tight or your socks leave a mark around your ankle or leg. If your legs only hurt when you are walking and the pain goes away when you stop, the problem may not be in the veins, but in the arteries. It’s important to distinguish between the two because the causes and the treatments are different. Either way, you should see your primary care provider for an accurate diagnosis.
If you have varicose veins it’s likely that your mother or father or both also had them. Add a job that keeps you on your feet all day and your odds of developing them increase even more.
Varicose vein risks
- Family history
- Increasing age, which can cause wear and tear on valves
- Gender. Women more likely to develop, but men can too
- Obesity
- Standing or sitting for long periods
Pregnancy and varicose veins
Dr. Asbjornsen recommends that pregnant women in a high-risk category wear compression stockings for the first trimester — from the moment they discover they’re pregnant. The stockings continually squeeze your legs so that blood can flow more efficiently. The first trimester of the first pregnancy is when leaks that can lead to varicose veins often begin even if there are no telltale signs, said Dr. Asbjornsen. All pregnant women can benefit from wearing compression stockings, but especially high-risk women.
Jane said she continues to wear her stockings at work, more out of habit than anything, but also because she’s still on her feet a lot. For many years she also had to deal with recurring ulcers on her lower left leg. Knock on wood, she has been ulcer free for ten months. And she was delighted to report that this past summer (2011) she wore a skirt for the first time in decades!


Thank you so much, this tip will save my life. I am sedentary and have trouble losing weight.
I heard you on Maine Calling and you mentioned a podcast on vein health, but I can’t seem to find it on your website.
Here’s the link Deb: http://dianeatwood.com/vein-treatments-spider-varicose-deep-vein-thrombosis/
Very nice blog on varicose veins thanks for sharing such information keep up share things like that.
I love how you explained the symptoms of varicose veins is that your legs feel tired and heavy at about mid-afternoon. A lot of people probably don’t know anything about this disease and so listing the symptoms is very helpful. Thank you for bringing this disease to mine and other peoples’ attention.
I came upon this piece of information about the Modern techniques for treating varicose veins. A great piece of work. Keep us updated. Thank you.
Health is achieved by balancing the body, mind, and spirit and medication provides a way to achieve this balance. Medication results in many physiological changes including the reduction of inflammation in the body. Several studies have proved that mindfulness meditation can be a useful treatment of pain syndromes. Meditation has proved that through the regular practice of meditation one can change the perception of pain. Meditation develops our capacity for detached observation and helps us to spate our experience of physical sensations from the pain and emotions that are generated in reaction to those sensations.