
Jashina / Pixabay
More tired than usual? Losing hair? Feeling low? Irritable? Shedding pounds when you’re not even trying? Or dieting like crazy and the scale won’t budge? These are all symptoms of thyroid disease.
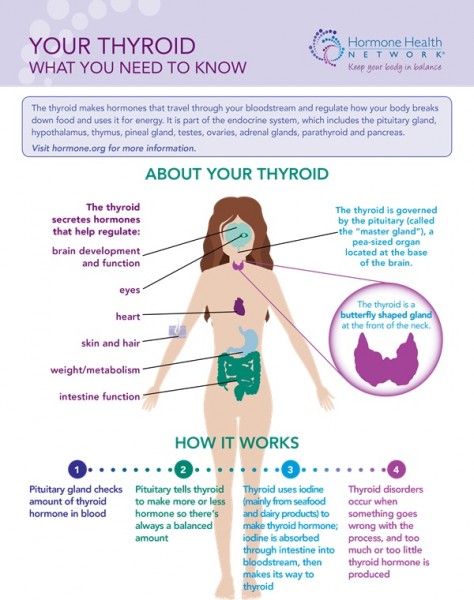
The thyroid, which is in the front of the neck above the collarbone, is a critical organ. When it’s working right it provides energy to nearly every part of the body. It gets its marching orders from the pituitary gland, which sits in the base of the brain. The pituitary signals the thyroid to get to work by releasing a thyroid stimulating hormone known as TSH.
When it receives the signal, the thyroid produces two primary hormones — T4 (Thyroxine) and T3 (Triiodothyronine). Under normal circumstances, these thyroid hormones circulate in the bloodstream and help regulate a host of important functions — breathing, heart rate, body temperature, menstrual cycles and more.
If the pituitary gland senses that more thyroid hormone is needed, it sends a stronger signal in the form of more TSH. If it senses too much thyroid hormone, it cuts back on TSH. When your body makes too much thyroid hormone, you have hyperthyroidism or an overactive thyroid. Too little is hypothyroidism or an underactive thyroid.
Hyperthyroid (overactive)
An overactive thyroid kind of puts your body into overdrive. Symptoms include:
- Sudden weight loss
- Rapid or irregular heartbeat or palpitations
- Nervousness
- Irritability
- Trembling, usually in the hands
- Muscle weakness
- Sensitivity to heat
- Difficulty sleeping
- Fatigue
- Changes in bowel habits — especially diarrhea or the need to go more often
- Changes in menstrual cycle
- Swelling in the base of the neck, which could mean the thyroid gland is enlarged (goiter)
- Bulging eyes
Hyperthyroidism is more likely to happen to women between the ages of 20 and 40. Someone who is older may hardly notice any signs. And if he/she is taking a beta blocker it can hide symptoms.
I spoke to a woman who had only one symptom. Extreme weight loss. She went from 240 pounds to 96 pounds in the course of a year. Her doctor was working her up for cancer when she went into multisystem organ failure and nearly died. The real diagnosis was Grave’s disease, an autoimmune disorder that is the most common cause of hyperthyroidism. It happens when the immune system produces antibodies that instead of protecting against various germs, tell the thyroid to produce too much thyroid hormone.
Thyroid nodules can also cause an overactive thyroid, as can an inflamed thyroid (thyroiditis). If thyroiditis is the cause, it may resolve on its own and careful monitoring for a few months may be all that’s needed. If it’s true hyperthyroidism, no matter what the cause, it does have to be treated.
Treating hyperthyroidism
Treatment options vary depending on things like the severity of the disease, your age, overall health and personal preference. It may not be cured, but thyroid function can be brought back to normal. More common treatments include:
- Radioactive iodine treatments
- Medications
- Surgery
Complementary and alternative approaches may also help relieve some symptoms. Make sure your medical providers know what you’re doing/taking. You want to make sure one treatment doesn’t interfere in some way with another.
Hypothyroid (underactive)
Hypothyroidism is far more common than hyperthyroidism — it affects about 10 million people in the United States. The most common cause is another autoimmune disorder. This one is called Hashimoto’s disease. A different set of antibodies attack the thyroid gland and cause it to become inflamed and unable to produce enough thyroid hormone. It tends to run in families, and like Grave’s is more common in women. Risk increases with age.
[Tweet “Diagnosing thyroid disease can be complicated”]
When you have an underactive thyroid, some functions tend to slow down. But it can be challenging to get a diagnosis. There is a long list of possible symptoms and many are linked to other diseases. And some people may have such mild symptoms, no one suspects a thyroid problem. Here are some of the more common symptoms:
- Feeling tired even after a good night’s sleep.
- Depression
- Weight gain or trouble losing weight
- Feeling unusually cold
- Constipation
- Dry skin
- Hair loss
- Hoarseness
- Muscle cramps
- Changes in menstrual cycle
- Memory problems
Some symptoms may be managed with lifestyle changes — less stress, better nutrition, more physical activity – but most people with an underactive thyroid end up needing medication to replace the missing thyroid hormone.
The key with thyroid disease is to make sure it is well controlled, particularly during pregnancy. Whatever the treatment, it’s important to continually monitor thyroid hormone levels. “Replacement thyroid hormone [must be] properly adjusted,” says endocrinologist Dr. Christine Twining, “because we don’t expect it will just be one dose and you stay on that dose forever.” Dr. Twining is the Medical Director of
Dr. Twining is the Medical Director of Maine Medical Partners Center for Endocrinology and Diabetes in Scarborough, Maine.
Getting a diagnosis
A simple blood test that measures TSH levels can pick up a thyroid disorder, but for some people, get anything but simple. I heard from a woman who said it took nearly 10 years to get a diagnosis. “Ten years of experiencing almost every hypothyroid symptom there is even though my TSH level was within the “normal” range,” she told me.
Dr. Twining says 95 percent of the time, TSH levels will give an accurate picture, but … “There’s a small group of people who have a pituitary problem, so their central signaling pathway isn’t working right,” she explains. “They may appear to have a normal TSH but if you check their free thyroxine ( free T4) levels they would be low. They have a normal signal, but they have low thyroid hormone levels in their body because their body is not appropriately increasing the signal as it should.”
Common blood tests
- TSH
- Measures the amount of TSH (thyroid stimulating hormone). Levels decrease with hyperthyroidism and increase with hypothyroidism.
- T4 — Free T4 (FT4) and Free T4 Index (FT4I or FTI)
- Measures the amount of T4 (thyroid hormone).
- Will be high with hyperthyroidism and low with hypothyroidism.
- T3
- Measures the amount of T3 (thyroid hormone).
- Usually used to diagnose hyperthyroidism.
You might also want to be tested for the antibodies that cause Hashimoto’s (hypothyroid) or Grave’s Disease (hyperthyroid). “Knowing [that you have either disease] won’t change the course of treatment,” says Dr. Twining, “but it would give us more information about the pattern. “Someone might have mild hypothyroidism that gets picked up on a blood test. If you check and find out that it’s caused by an antibody, you know to tell the patient this is likely to progress.”
And because both autoimmune diseases tend to run in families, knowing that you carry antibodies will be useful information for the rest of your family members.
What about screening tests?
The U.S. Preventive Services Task Force does not recommend routine thyroid screening for non-pregnant adults who have no symptoms. It does encourage doctors to be aware of subtle signs of thyroid disease, especially in people who may be at high risk.
- Elderly people
- Postpartum women
- People who have been exposed to radiation
- People with Down syndrome
Dr. Twining adds family history to the list. “The jury is out on intervals or whether the whole population should be screened for hypothyroidism,” she says, “but anybody with a family history of either hyper- or hypothyroidism should at least be screened — just a TSH and a thyroid physical exam.”
The thyroid patients I spoke with all said it’s important for people to listen to their bodies and their intuition. And to speak up if they think they might have a thyroid problem. “Thyroid patients need to be their own advocates,” said one woman, “and research, research, research!”
More information
If you’d like information about thyroid nodules, read my post If you have a thyroid nodule does it mean cancer?
If you’re looking for information about thyroid cancer, read my post Some important information about thyroid cancer.
I also compiled a list of resources based on recommendations from Dr. Twining and several people with thyroid disease.
ThyCa: Thyroid Cancer Survivors’ Association, Inc.
This post was originally published on the Advantage Home Care blog, which I also write.

Great PSA, Diane. My mother had Graves disease, as does a friend, and I continue to be surprised at the number of women I know who have hypothyroidism. One more thing to be vigilant about!
I know! And I was shocked by the long, long list of symptoms.
I have hypothyroidism and I got very sick before I was diagnosed. I still have thin hair and trouble losing weight, but the medication is easy to take and I’ve been able to do a lot of things I never thought I could.
Hi Jo Ann! I was transcribing your interview earlier this week. Were your ears burning? Should get the post written soon. I’m glad you’re doing better.