I’m religious about getting my annual mammogram. That’s because I have a history of fibrocystic disease and in my 20s had a fibroadenoma (benign tumor) removed from my right breast. Every year, I worry that something not so benign will show up and every year I sigh with relief when I get a letter saying everything is normal. Not this year. Instead, I got a phone call from the Mammography Department at Mercy Hospital. The radiologist wanted me to come back for additional views. My heart sank.
My husband Barry took time off from work so he could go with me. If there was any bad news to be delivered, I didn’t want to hear it alone. Renee, the kind and wonderful mammography tech who had done my screening mammogram told me she was going to take some magnification views so they could look at an area in my right breast more closely.
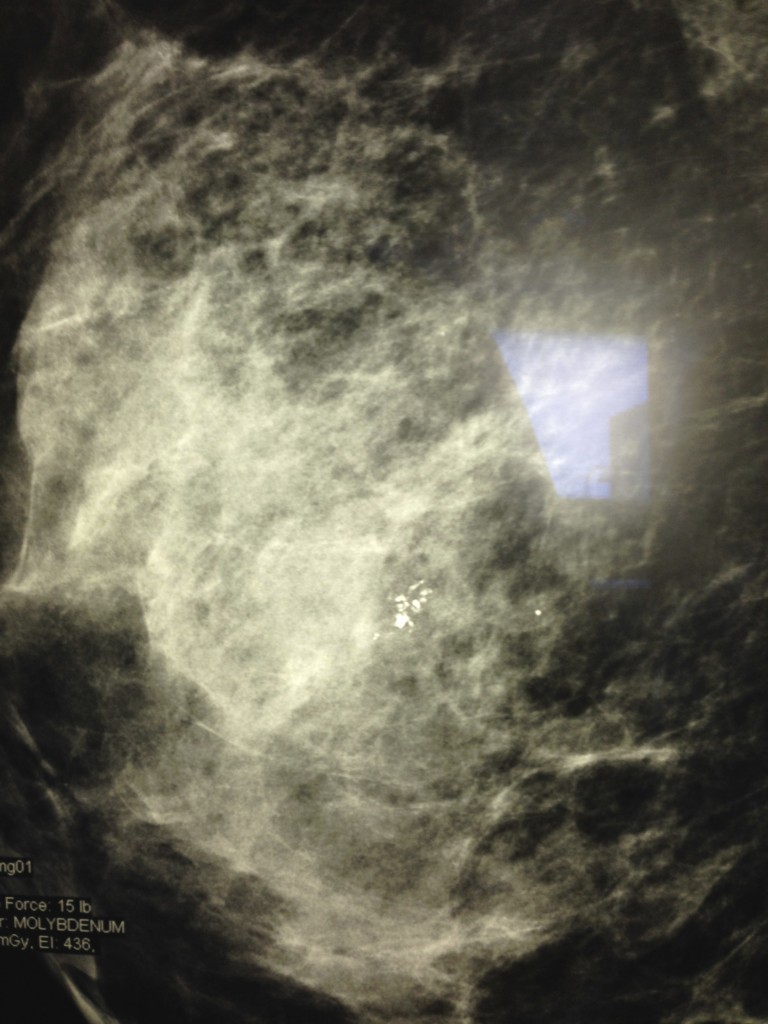
After she was done, Barry and I were ushered into the viewing room to talk with the radiologist, who pointed out a sprinkling of tiny white dots near the middle of my mammogram and explained that they were microcalcifications. Some of them looked normal, but others could go either way. Either way? I tried to remain calm and stared at the image intently. You can look too. The picture at the beginning of this post is a copy of the magnified view.
While he talked, I studied the dots and saw what he meant. Some seemed symmetrical, but a patch of them looked irregular. What should I do? I asked. His response was that I could watch and wait or get it biopsied. I’m generally not good at watching and waiting for anything and in this instance, there was no way I’d choose that option. I need to know what I’m dealing with I told him. Let’s get it biopsied.
The biopsy was not fun, but everything went smoothly and it didn’t take as long or hurt nearly as much as I expected. Thank goodness for small favors or in my case, for an average-sized breast with calcifications in an easy to access location. I had a stereotactic biopsy and plan to go into more detail about the procedure in a future post. I’m also more than happy to answer your questions if you have any.
Diagnosis: DCIS
Three days after the biopsy, my primary care doctor called to tell me it was positive for ductal carcinoma in situ or DCIS. Surprisingly, I didn’t fall apart. In that moment I was calm and ready to take action. The radiologist had mentioned DCIS, so I had researched it quite a bit and had “my plan” in place. If I needed surgery, my first choice was Breast Care Specialists at Mercy. Because I did Mercy’s marketing and public relations for many years, I knew them well and felt confident I would be in good hands. That said, I am a firm believer in second opinions and got one from Dr. Dixie Mills, who is currently director of breast services at Harvard Vanguard Medical Associates in Boston and at one time was the medical director at the Dr. Susan Love Research Foundation.
Before I continue my personal story, I want to explain some of the things I’ve learned about DCIS. It’s considered a stage 0 breast cancer that is not life-threatening and potentially 100 percent curable. Some health experts refer to it as a noninvasive precancer. Abnormal cells are inside the milk ducts and have not spread to surrounding breast tissues. If any do spread, it’s considered invasive cancer. Nearly all invasive breast cancer starts out as DCIS, but not all DCIS goes on to become invasive. The problem is there is no tried and true way to know which ones will evolve. That’s why treatment is usually recommended, beginning with surgery and possibly including radiation therapy and tamoxifen, a hormone therapy used to treat invasive breast cancer and DCIS that test positive for estrogen receptors.
According to the American Cancer Society, about 60,000 cases of DCIS are diagnosed in the United States each year, accounting for about one out of every five new breast cancer cases. (Although it’s unusual, men can also get DCIS.) Finding a lump is pretty rare with DCIS; most of the time it’s discovered on a mammogram.
There are two main reasons there are so many cases of DCIS and why the number continues to grow:
- People are living longer and, as we age, our risk of breast cancer increases.
- More people are getting mammograms and the quality of the mammograms has improved. With better screening, more cancers are being spotted early.
Meeting with the breast surgeon
A few days after I got my biopsy results, my husband and I met with the surgeon, Dr. Suzanne Hoekstra. She explained that the biopsy had removed some, but not all of the calcifications. What was left appeared quite small, which relieved me greatly — for a few seconds. Because on the flip side, what they could see on the mammogram taken after the biopsy might only be the tip of the iceberg.
We agreed that a lumpectomy was the best next step and we’d wait for the pathology results before deciding about any further treatment. It was really hard not to flip out then and there.
One the day of my surgery, I was essentially on autopilot and more afraid of the wire localization procedure I had to have than going to the operating room. Because there was no lump to feel, just microcalcifications, Dr. Hoekstra needed something to lead the way to the abnormal cells.
After I had checked in at the outpatient surgery department, Dr. Hoekstra’s nurse Elizabeth Huebener bundled me up in a wheelchair and delivered me to the mammography department where Renee took more x-rays and using them as a guide, Dr. Hank Talarico, the radiologist who had also done my biopsy, inserted a fine wire into my breast. I sat there with my breast squeezed between two plates staring out the window trying not to focus on what was going on as he inserted the wire. Suddenly, tears were streaming down my face. He was as kind and gentle as he could be. It didn’t even hurt, just stung a little, but I felt invaded and helpless and scared. As soon as it was done, Renee and Elizabeth sprang into action and gave me comfort — there is nothing better than arms wrapped around you at a moment like that.
My other comforts were Barry and my sister Becky, who watched over and entertained me (and everyone else) throughout the long morning. Humor is right up there with hugging.
Going into surgery and later the recovery room are mostly a blur. Before I knew it, I was on my way home, my chest completely enveloped by an ace bandage. More comfort was waiting for me when I arrived — my sister Debi with a steaming bowl of homemade chicken soup loaded with fresh vegetables from her garden.
The surgery was on Friday, September 19, 2014. The following Tuesday, Dr. Hoekstra called to tell me she got all of the DCIS, which turned out to be about the same size as on the mammogram, and wide margins of normal breast tissue. It was the best possible news.
A few days later we met in her office and went over my risks and agreed that because the DCIS was small — about 5 mm at its largest — and the margins of normal tissue so large — from 4 mm to about one centimeter — I could say no to radiation therapy treatments. It’s a decision that can’t be made lightly and not one that all women would choose, but after discussing it with both Dr. Hoekstra and Dr. Mills, it seemed like the right choice for me.
There is so much more I could say about my experience and what I’ve learned about DCIS and I expect I will in future posts. If you learn one thing from this blog post, I hope it is that if you’re due for a mammogram, don’t put it off.
American Cancer Society mammography guidelines
- Yearly mammograms are recommended starting at age 40 and continuing for as long as a woman is in good health
- Clinical breast exam (CBE) about every 3 years for women in their 20s and 30s and every year for women 40 and over
- Women should know how their breasts normally look and feel and report any breast change promptly to their healthcare provider. Breast self-exam (BSE) is an option for women starting in their 20s.
Some women — because of their family history, a genetic tendency, or certain other factors — should be screened with MRI in addition to mammograms. (The number of women who fall into this category is small: less than 2% of all the women in the US.) Talk with your doctor about your history and whether you should have additional tests at an earlier age.
Paying for a mammogram
If you’re worried about paying for a mammogram, the Maine CDC Breast and Cervical Health Program offers free mammography services to women who are eligible according to age, income and insurance coverage. For more information, visit the Maine CDC website or call 1-800-350-5180.
The Affordable Care Act mandates that screening mammograms be covered by insurance with no co-pays or deductibles. On the American Cancer Society website, you can read an overview of the various laws that require private health plans, Medicaid, and Medicare to cover early detection services for breast cancer screening.
Gratitude
I am filled with gratitude that my mammogram picked up the microcalcifications — they weren’t there the year before and they could have been something else by next year. I happen to have some risk factors for breast cancer — I had my children in my late 30s, I’m over 60 and I have a history of benign breast disease. I’m now at an increased risk of both DCIS and invasive breast cancer. I will be followed closely by Dr. Hoekstra — and if either rears its ugly head, hopefully, we’ll catch it early again.
I’d never heard of DCIS before and I’m discovering that neither have a lot of other women. If you have any questions or comments, don’t hesitate to get in touch. You can leave a comment below or send me an email.
I’d like to finish this post by saying thank you to everyone who helped me along the way — most of them at Mercy. There wasn’t a single person who wasn’t professional and kind, but I didn’t get everybody’s names. Those I would especially like to thank include Renee and Dr. Talarico in Radiology, Dr. Hoekstra and Elizabeth at Breast Care Specialists, Lauren, my pre and post-op nurse, and Dr. Brian McAllister, the anesthesiologist. Also, thank you to Dr. Mills and, of course, to Becky and Barry!



Diane….just read your account of your mammogram up to and past surgery. Dr Talarico is awesome for reading mammograms and Dr Hoeckstra is a perfectionist from what I heard when I worked at Mercy. I retired from Nuclear Medicine this past August 29th, and Paula and I now live in Apopka, FL near our daughter. I wish you well and a long and happy life. I am happy to hear things are going well for you. The Breast Health Center at Mercy is truly an awesome group of professionals.
Chuck Keogh
Wow Chuck — you’re retired! You’re not bored down there in sunny Florida are you? You probably get up every morning and say, “What fun thing can we do today?” Enjoy every moment!
Diane,
THANK YOU so much for sharing this important story. A great reminder of why yearly mammograms are SO important. Having had a fibroadenoma discovered during my baseline mammogram at age 35, I’ve been pretty faithful about screening as well, but I will remind myself of this story if there’s ever a year I think I can skip it “just this once.”
Jen
You are welcome Jen! Some guidelines recommend baseline at 50 and screening mammogram every two years, but American Cancer Society says 40 and every year. It’s confusing, but I think it’s important to know your personal risk factors — I was told benign breast disease, e.g., fibroadenoma was one, so always tried to have one yearly. Take care!
Hi Diane,
I am sorry you had to go through the worry and the procedure, but glad you caught it early in a routine mammogram and that you are bringing this important routine screening to people’s attention. Having a great support group of family and trusted health care providers helps more than anything when you have to deal with a scary diagnosis. I have discovered a few breast lumps through self exam and fortunately they turned out to be nothing of consequence. But the worry, in spite of a great support group, was difficult while waiting for tests and losing sleep makes it all seem worse.
To deal with worry while dealing with difficult situations I found lavender/chamomile tea (no caffeine) before bed helps reduce anxiety, and I am better able to sleep. This tea should not be consumed regularly. I have made my own, growing lavender and steeping a few flowers in a pot of tea, but it is available in stores.
Thank you for the reminder to have routine mammograms.
Betsy
Betsy, I apologize for not responsing sooner, but your comment slipped right by me. I’m so glad your lumps turned out to be nothing. As for the tea suggestion, I drink chamomile tea every morning. I’ve never tried it with lavendar, but I have some growing outside my kitchen, so now I can!
The screening mammogram is covered but the $100.00 to read the mammogram is not covered by the insurance. That hurts for many people and discouraged women from going. It all should be covered. Why pay for a test and not find out the results? I am a stage 1 invasive cancer survivor of almost 14 years. The wire locs is the pits. I also had Mercy breast center.
It’s all very frustating and confusing isn’t it Brenda? I agree about the wire localization. That’s when I felt my most vulnerable. I’m glad you’re doing fine!
i recently went thru a similar situation. Routine mammogram showed an abnormality. Follow-up of diagnostic mammogram and ultrasound, read by the radiologist who indicated I needed a needle biopsy. Ultrasound guided needle biopsy was performed and I was chipped in case there were questions on future mammograms. Met with surgeon after pathology report showed I had Stage 0 DCIS and lumpectomy was recommended. Day before lumpectomy, I had to go and get a radioactive seed implanted, instead of the wire you had, which was used as a marker to assist in locating the area to be removed. Seed was removed during lumpectomy. Very little discomfort thruout all the various procedures for the most part. My follow-up appt. was last week and he said he got clear margins and I don’t have breast cancer. He said no other surgery was necessary but did arrange for me to see an oncologist this week and said I will probably either be required to take Tamoxifen (I still have my uterus) or 6 weeks of radiation at 6 days a week. He also said they may just decide to do more frequent mammograms and watch it. I am 62 and don’t have many risk factors so I am thinking I would rather do the frequent mammograms rather than treatment which may cause other problems. Would appreciate hearing your thoughts on this?
Anne, I’d love to have a conversation with you about how I made my decision. There were several factors that went into it and my situation may not be the same as yours. Send me an email — diane@dianeatwood.com — if you want to talk and we can set something up. Deep breath!!
Hi it’s 2018 and I was wondering how you are doing now? Thanks, linda
Knock on wood, everything has been fine at my annual checkups. I’m always filled with anxiety for several days before, though. Thank you for asking.
Thank you for sharing this. I have the same diagnosis and facing the same surgery. It was comforting to read the steps of the procedure from someone who had gone through it. I am not quite as scared now. Just still afraid of the findings after but that can’t be predicted. I will just try to keep a positive attitude.
Jean, I’m so glad I could help even a little. I’ll be thinking of you.
Hello, thank you for sharing your story. I may be facing the same prognosis, have fibrocystic breasts and micro calcifications that look just like yours. Going for a biopsy next week. I am wondering how you are doing now, 2021? I am also wondering about how the lumpectomy is done, and what is the damage to the breast from the surgery? Did you have to have any plastic surgery afterwards? How much do they open the breast to get the lump out? Feeling afraid…
Hi there, can you send me an email? diane@dianeatwood.com. Thanks, Diane
Hello Diane!
Glad all is still A-okay with you and your breast health! Your post states perfectly each step I went through as well, including the scariness of that wire being put in! I had DCIS in 2011, had lumpectomy, then radiation, no Tamoxifen—have been clean ever since.
I wonder whether I should get the diagnostic mammogram each year, or if the screening mammo is fine since it’s been 7 years now. Just wondered what your docs have told you about 5 years out, if anything.
Continued good health to you!
Glad to hear everything is ok with you, too, Jean. I’ll be going for a 4-year checkup this summer and will ask about mammograms. For now, it’s scheduled and reviewed the same day I see my surgeon. So far, so good!
I just found out that I have an “area” that needs further review and I have a diagnostic mammogram scheduled for 23 May. My mother passed away from breast cancer in 1987 so I am scared to death. I have been reading up on the different stages of breast cancer and came across your article. Thank you for posting as I found it very informative. I am glad you are doing well.
Valerie,
It IS very scary. I’m glad that reading about my experience was helpful for you. I will be thinking of you. Let me know how things go. Diane
Diane, The post is very useful.Right at the time when I had to decide what to do.
Similar situation with DCIS in the left breast,and PCIS in right.
At 81 it is dilemma.
Do I need to go through ordeal of operation and treatment, while I still active and independent, with clear mine.
So far, I have tried to avoid not life’s threatening operations, because I scare to loose independence.
Confused and lost
I’m glad my story was helpful. It’s a lot to take in. I tried to get as much information as I could, including other medical opinions and then just had to make up my own mind about what felt right for me. I’ll be thinking of you.
Hello Diane,
I want to thank you for sharing your story. I am in a very similar situation right now. I am scheduled for stereotactic biopsy.
A bit about my history how it all started….. I am 47 year old and 17 years ago I felt a lump on my left breast after taking shower. I got so nervous and went for the mammogram. They sent me for a biopsy. They ended up removing the lump what they called fibroadenoma (benign tumor). It was confirmed it was not cancer but felt it should be removed because it could grow bigger. They recommended I should be getting my mammograms done every year after that. I will be honest, I did not follow up all the time consistently every year but recently for the past 4 years I have been doing so. When I had my mammogram done last year, they called me back to do an extra ultrasound because I have a lot cysts in both breasts. They concluded that all looks fine. Two weeks ago I asked my doctor to send me for the mammogram because I have not been feeling very well for the past few months. Having chest pains on my left side and arm/shoulder/neck pains. I even went to check my heart for any heart problems but it all came back my heart is all good. The pain still continues in my chest so I asked to get a mammogram done, I thought perhaps I have something wrong with my left breast. So they found microcalcifications in my left breast. They sent me for the second mammogram and I just got a call from the hospital that I need a biopsy. I am schedules for February 12, 2019, 2pm.
I am very nervous and stressed just because my body has not been well for the past 4 months. I have always been healthy and it’s just recently my body is not well. This adds a bit more anxiety and worry.
How did you feel? Did you feel any pains or aches before?
Your article truly calmed me down and made me feel a bit more positive. Thank you for sharing it and wishing you all the best.
Hi Diane,
i’m 73 and in pretty good shape, people think i’m 60 which i will be happy to take. Having said this, for 40 yrs i had normal mammograms, aug 2019 i had my first abnormal one. this totally floored me! The radiiologist and surgeon felt i could wait 6 months to see what was happening. There is no breast cancer, either on my mother or father’s side, none i ever heard of. This past feb 2020, I went for my 6 month check up and there were more microcalcifications. Went for a biop and it was DCIS stage 0 – this was scary and I read everything, I could get my hands on. I’m going to see the surgeon in two weeks and will have a consult with her. My questions to you are – should I have gone the first time I found out I had the microcalcifications?? Does the doctor decide what type of surgery you will get, lumpectomy or mestectomy (which i do not want)?? How soon does a woman have to get surgery when biop is given?? And does a lumpectomy hurt, esp with that wire localization thing???? I have tried to find these ansers on line but never came across anyone giving out info regarding these questions. Your article was very easy to follow and that’s why i am asking you the questions, esp before i go see the surgeon. I know we are all different, whereby, some people get radiaton or radiation and hormone therapy. I don’t know how long i would have to wait to get on with my life bc I am active. Also don’t know how long radiation would be. These are all questions I have regarding this situation. ugh at 73. thank you so much – glad you are doing well
Hi, I was diagnosed with DCIS stage 0. I had the surgery to remove any remaining cancer (partial lumpectomy) and none were found after the second surgery. They did recommend radiation treatment and hormone therapy. I can’t see having radiation treatment when having treatment as opposed to not having treatment is the same percentage of it returning. I was told 17%. They also recommended hormone therapy- anastrozole for 5 years. I am not a fan of that due to the horrible side effects, I have Lupus and I already have terrible joint pain in my knees and hands, I don’t need anything else negatively affecting my bones. It looks like my surgery which I already had will have to be my only treatment along with increasing my exercise back to 1 hour a day for 5 to 6 days a week, eating healthy, and increasing my praying to God. I asked for healing before my surgery and the pathology report came back with no cancer. If it were not for the Lupus I would consider the hormone therapy. It just seems DCIS stage 0 is being treated as if you have breast cancer. Diane, how are you doing?
Hi Chere. knock on wood and fingers crossed, I’m doing ok. My surgery was 7 years ago last September, and every year I get a mammogram and see my breast cancer specialist. It wasn’t an easy decision to only have a lumpectomy and no radiation or hormone therapy, but I did a ton of research and got more than one medical opinion. If I’d been younger I might have made a different decision, but I was in my mid-60s then. In case you didn’t see them, I wrote some additional blog posts on the subject: https://dianeatwood.com/stage-0-breast-cancer-treatment/ and https://dianeatwood.com/dcis-five-year-checkup/. Take care!
Hi there. I am at the beginning of this journey and have been worried to the point of feeling like I’m holding my breath fearing the worst. I would like to tell you that after reading about your experience, I feel like I can let out a breath of relief. Thank you so so much for sharing this.
Hello,
I too have DCIS. I chose lumpectomy. The pathology report was the best of outcomes with no border invasion; small DCIS area of one to less than five cm’s. I am 70 and not feeling comfortable with the decision making of my oncologist and surgeon to undertake radiation and hormone therapy. Most DCIS studies I have found do not include women over 70. I am conflicted and feeling very alone without the support of my health care team. I am pondering taking radiation only or no treatment with the exception of follow up mammograms. When I try to discuss this with my health care team I am met with silence. Any suggestions?
Great article! I hope you are still doing ok?