Cynthia, who’s now 59, experienced her first floater in her eye when she was 13.
And I remember distinctly because I saw this thing that looked like it belonged underneath a microscope, like a little amoeba. I asked my mom about it and she said, “Oh, it’s nothing, it’s just a floater.
Cynthia
Her eye doctor agreed. Floaters aren’t usually a big deal, but they can be an early warning sign of a retinal tear or a detachment, especially, later in life.
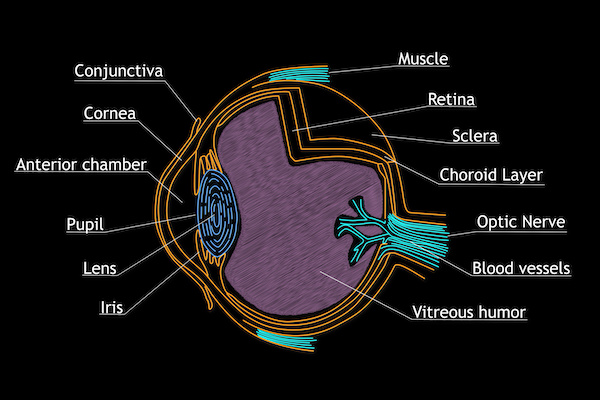
Our eyes are filled with a gel-like substance called the vitreous, which contains tiny fibers that are attached to the retina. The retina is a thin layer of tissue that covers about 65% of the back of the eye. It receives light and changes it into signals that it sends to the brain — an important part of us being able to see.
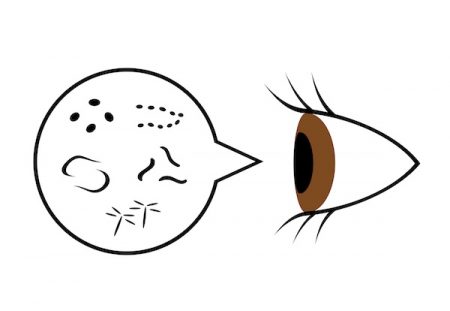
Floaters are little clumps of the gel inside your eye. What you see are shadows of the clumps cast on the retina. As we get older, the gel shrinks and the tiny fibers begin to pull on the retina.
Sometimes when a fiber is pulling on the retina the fiber breaks. That’s called a vitreous detachment or a posterior vitreous detachment (PVD). It’s not a serious issue, and no treatment is usually necessary. Age is the primary risk factor for PVD, but additional ones are recent eye surgery, such as cataract removal and myopia, or nearsightedness. Dr. Aaron Parnes, a retina specialist with Eyecare Medical Group, explains the role that myopia plays.
In a highly myopic or nearsighted eye, the eye itself is longer. That elongation causes you to need glasses in order to focus the light farther back than would normally be needed. That elongation also causes the retina to be stretched out — it has to cover a larger surface area.
Dr. Aaron Parnes, retina specialist, Eyecare Medical Group, Portland, Maine
Cynthia is at increased risk of retinal problems because she is nearsighted. She started wearing glasses when she was 12-years-old and ever since her first one at age 13, has gotten quite used to seeing floaters. In early March she had an entirely new experience. She began to see flashing lights in the periphery of her left eye.
It was absolutely terrifying. These bright flashes of light that if you were looking at the sky, look like a lightning bolt that flashes and disappears. And then you move your eye and it flashes again and it disappears. I’d never seen this, so I went to an eye doctor and he said what I was seeing was a fiber tugging on the retina.
Cynthia
You might think you’d feel it if something was tugging on your retina, but it has no pain sensors, so you see flashing lights instead. That’s why it’s important to pay attention to light flashes or other clues your eye might be sending you that something potentially serious is going on.
Dr. Parnes emphasizes the importance of recognizing the early warning signs.
Initially, you’ll have floaters, black dots, or flashes of light in your vision. Floaters mean either there is bleeding or the gel has shifted around. A flash comes as an arc of light on the side of your vision and goes away immediately. There can be multiple flashes at once. They indicate pulling on the retina.
Dr. Aaron Parnes
Pulling on the retina can cause PVD, but it could also lead to a retinal tear and unfortunately, that’s what ended up happening to Cynthia. She was scheduled to see her eye doctor a month after he first saw her, but after experiencing three weeks of continuous flashing lights, something more dramatic occurred.
On the morning of March 26. I was on my computer and these flashes got super bright, super intense and they arced over the entire top of my eye. About 15 minutes later, I saw this thing move across my eye that was like a cloud. I thought, oh my god, that is not good. This big, bulky thing was moving across my eye, and then I saw a darker thing that looked like an octopus flat across my eye, which dropped thousands of little floaters on me.
This was the height of COVID, round one, but the doctor saw me immediately. He examined my eye and said, “Well, the bad news is you have a retinal tear. The good news is it’s not a retinal detachment yet.
Cynthia
Fortunately, the tear could be treated with a laser, which uses heat to seal around the tear and decrease the likelihood of a detached retina.
It took about 15 minutes. The eye doctor had on this weird virtual reality headset and the laser in his hand. He had me torque my head so he could laser in on the spot, and 15 minutes later, he had sealed the hole. I couldn’t see anything for about 10 minutes after that because the light was so blinding that my brain had to get used to that happening. We left and went home and I looked like somebody hit me in the face with a baseball bat because my eye was solid red.
Cynthia
The laser sealed the tear in Cynthia’s retina, but the afternoon after her treatment, another black “octopus” streaked across her vision. Back she went to the eye doctor, who discovered that when the tear occurred it nicked a blood vessel. Several months later, Cynthia said it seems as if she is looking through a snow globe.
My vision is actually fine. My vision has not changed, but I have a lot of debris in there — floaters and cloudy stuff, and also a lot of blood in the eye because of the nicked blood vessel. I’m hoping that eventually, more blood will get reabsorbed and I won’t have as much debris floating around in my left eye.
Cynthia
It could be a year before her eye clears up and the debris may not all go away. And once you’ve started the PVD process in one eye, it’s likely to happen in the other eye as well within a year. Sure enough, Cynthia has already started noticing symptoms.
I started having flashing in my right eye, and I don’t honestly know how long has it been going on. I happened to notice it when I was going up a staircase where there’s a blank wall. Then it was really easy to see. But it’s really, really far back in the periphery.
Cynthia
Because of the experience with her left eye, Cynthia knows that the flashes in her right eye indicate that there is pulling going on. She’s trying to take a calm approach to the idea that she might have another retinal tear. Every day she meditates.
As part of my meditation, I always say to myself, I only have a 10% chance of it happening again, I only have a 10% chance of this happening again, let’s focus on that.
Cynthia
The biggest risk she faces is having a retinal detachment, which is what happens if you have a tear and fluid leaks out under the retina. Serious business, says Dr. Parnes.
If the fluid does go through the retinal tear and the retina separates from the back of the eye, you’ll see a shadow or curtain come over your vision. It starts in one field of your view and eventually, will envelop the entire field. Your vision in that eye will be darkened. When the retina is detached, you can’t just laser it back. You need surgery. The usual procedure is vitrectomy. We remove the gel that fills the eye which removes the pulling on the tear or tears. Then we have to reattach the retina. We usually use a gas bubble to push it back into place. Then we apply a laser to create a scar just like we would if the retina was already attached and there was just a tear there. You usually need to position your head either facing down or facing one way or the other depending on where you want the bubble to push. As the laser scars down and seals everything in place, it keeps the retina attached over three weeks to two months, the bubble slowly dissolves and we keep a close watch to see that the retina remains attached. The healing process is long, more of a marathon than a sprint.
Dr. Parnes
As I mentioned earlier, the biggest risks associated with torn or detached retinas are age ( a PVD is more likely to happen after age 60), being near-sighted, or having recent eye surgery. Trauma to the eye can also increase your risk, and having an issue in one eye increases your risk in your other eye.
Paying attention to your eyes is the most important thing you can do to prevent more serious problems, says Dr. Parnes.
if you have symptoms, don’t ignore them. If flashes or floaters are occurring you should get a dilated eye exam, preferably within a day or so, because it could mean the gel has separated. In most people, the gel can separate and not create a tear or a detachment, but you can’t tell without getting an exam. So getting examined sooner when you have symptoms is a good idea.
Dr. Parnes
And don’t forget your routine eye exams. Cynthia couldn’t agree more. She never expected to become a retinal expert herself, but it happened. Almost overnight. And one thing that has caught her attention is how easily some people dismiss what’s going on with their eyes.
I got to know the eye doctor’s office pretty well, and they said that some people are so bodily unaware that they come in and their retinas are almost completely detached, which means they’ve had this black curtain over their eye. If you see a heavy drape moving across your vision or down from the top or up from the bottom you should know you have a problem. Get to the eye doctor, and also go if you notice a big floater that’s new or a lot of floaters that happen all of a sudden.
Cynthia
You may not be able to prevent torn or detached retina, but the earlier you catch them the more likely you’ll avoid more serious issues later on.
Cynthia has one final suggestion to help us all be more aware of our eyes. She’s added something to her morning routine that she says is quick and easy — you could even do it while you’re brushing your teeth. She covers one eye and takes a close look at the other, rolling it around and making sure she doesn’t see any floaters, flashes, dark curtains, or anything else that’s unusual. She does the same with her other eye, finishes brushing her teeth, and moves on with her day (and her daily meditation). I hope she doesn’t run into any more problems. Seems like she’s had enough this year.



Leave A Comment